The four key concepts that form the foundation for the nursing profession are person, environment, health and nursing. These concepts examine the primary doctrines of nursing practice. They also form the ground through which individuals should be examined and treated within the nursing profession. This paper looks at the application of these four concepts to the comfort theory of nursing.
Introduction
Various events in the course of the twentieth century led to the creation of the comfort theory. In the period between 1900 and 1923, the nursing profession developed a key interest in the importance of morality in their field. In the several decades that followed, until 1960, the profession was involved in the formulation of strategies that would help to achieve various aspects of health care (Kolcaba, 1994). Later, the nursing profession emphasized on physical aspects of care with focus on emotional comfort. The comfort theory was developed in the 1990s to address various health care concerns including pain management, child birth, end of life and palliative care and discomfort diagnosis (Kolcaba, 1995).
Background
Katharine Kolcaba developed the comfort theory in the 1990s. “The comfort theory is categorized as a middle range theory for health practice, education, and research since it can enhance comfort in the provision of health care” (Kolcaba, Tilton, & Drouin, 2006). Katharine was born in Cleveland, Ohio in 1944 (Malinowski & Leeseberg, 2002). She pursued a diploma in nursing at St. Luke’s Hospital School of Nursing in 1965 and later proceeded to Case Western Reserve University. She graduated from the university’s Frances Payne Bolton School of Nursing in 1987, and ten years later, she obtained her doctorate in nursing, as well as, her certification as a specialist in clinical nursing. Katharine specializes in various nursing fields including “nursing research, nursing theory, gerontology, comfort studies, instrument development, and end of life and long term care interventions” (Kolcaba & Wilson, 2002).
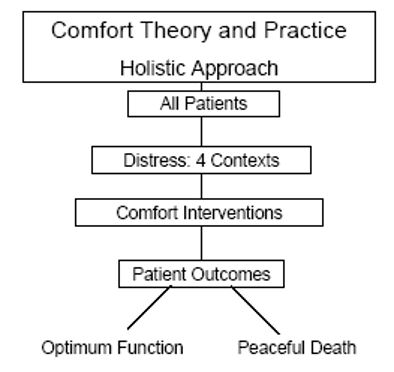
“The comfort theory provides a vision for holistic care and research, which supports clinical decision making in the management of pain” (Kolcaba, 1995). The comfort theory provides care givers with an understanding of nursing care. In addition, patients can understand its practice and their families can be an essential part in the implementation of the theory. The comfort theory is applicable to a variety of patients including those seeking to achieve their previous functionality levels, those going through strenuous therapies, and those who want to die in a noble manner (Morse, Bottorff, & Hutchinson, 1994).
Theory description
The foundation of the comfort theory is based on the development of a concept analysis that assessed various nursing disciplines including medicine, nursing, psychology, psychiatry, ergonomics, and English. These helped in the development of three types of comforts, four therapeutic contexts, and a taxonomic arrangement that could be used for examination, analysis, and evaluation of patient comfort (Pope, 1995). The three forms of comfort include relief, ease and transcendence while the contexts that demand provision of comfort in patient care include sociocultural, environmental, physical, and psychospiritual frameworks. One of the examples provided by Kolcaba about comfort care is the administration of prescribed analgesia to relieve postoperative pain. The comfort theory also proposes that patients experience comfort, in the sense of ease, if they feel contented, as in the case of addressing patient anxiety. The aspect of transcendence focuses on the provision of comfort so that patients can overcome their challenges. The holistic approach of the comfort theory and practice is shown in figure 1 below.
Evaluation
The comfort theory describes comfort as a direct, sought-after result of nursing care (Walker, 2002). It involves institutional integrity, which comprises standards, economic strength, and the entirety of health care institutions at a local, regional, and national level. The theory also addresses the provision of favorable policies and protocols that determine the institutional procedures involved when handling evidence regarding the health care needs of a patient. The comfort theory identifies various intervening variables, which are described as those aspects that care givers have little control over such as prognosis, financial well-being, and scope of moral support, among others (Walker, 2002).
The comfort theory also describes the four meta-paradigm concepts of nursing. First, nursing is depicted as the practice of examining the comfort needs of the patient. This concept also involves the development and implementation of necessary interventions, as well as, assessment of patient comfort after implementation of the interventions. Nursing also entails the deliberate evaluation of comfort needs, the planning of possible comfort actions that can attend to the identified needs, and the re-evaluation of comfort levels following their implementation. Evaluation can be objective or subjective. Objective assessment involves the inspection of injury healing while the latter involves an interaction with the patient in order to identify their level of comfort (Wang & Keck, 2004).
The comfort theory describes the concept of health as optimal functioning of the individual’s physical, social and metal functions. The opinions of the patient, family, or community form the basis for the assessment of the patient’s health. The person concept looks at the assessment of individuals with respect to their duty and relationships within a society. The concept also views the needs of individuals and the role of nursing practice in addressing them. The comfort theory satisfies this requirement by considering patients as individuals, families, institutions or communities that require health care services (March & McCormack, 2009). The environment concept of nursing holds that individual and collective health is influenced by both internal and external factors. The comfort theory seeks to provide a positive nursing environment by considering the aspects of the patient, family, or surroundings that can be controlled by either nurses or families to improve comfort (March & McCormack, 2009).
Application
The theoretical framework of Katharine’s comfort theory impacts the work and thought of health care providers in the provision of various types of comfort care including technical, coaching and comforting care. Technical care involves pain relief, positioning, and monitoring, while coaching care involves the relief of anxiety, provision of information, encouragement, and planning for recovery. Coaching, on the other hand, refers to various things that make patients and families feel cared for, supported and associated. Provision of comfort can be in the form of listening to patients’ concerns, providing reassurance, or providing medication to ease the pain (Kolcaba, 1995).
An example of the application of comfort to physical pain or physiologic problems involves the use of Opioid for nonstop pain as a relief strategy. An example of easing pain involves the elevation of a leg for edema patients, while transcendence can be portrayed through coaching to manage labor pains. In the environmental context, pain relief involves repositioning due to immobility, easing involves the use of distractions such as music during a procedure, while transcendence involves religious practice or rituals to calm the mind (Kolcaba, 1995).
References
Kolcaba, K. Y. (1994). A theory of holistic comfort for nursing. Journal of Advanced Nursing, 19, 1178-1184.
Kolcaba, K. Y. (1995). The art of comfort care. Journal of Nursing Scholarship, 27(4), 287-289.
Kolcaba, K., & Wilson, L. (2002). Comfort care: a framework for perianesthesia nursing. Journal of PeriAnesthesia Nursing, 17 (2), 102-114.
Kolcaba, K., Tilton, C., & Drouin, C. (2006). Comfort theory: A unifying framework to enhance the practice environment. The Journal of Nursing Administration 36(11), 538-543.
Malinowski, A., & Leeseberg Stamler, L. (2002). Comfort: exploration of the concept in nursing. Journal of Advanced Nursing, 39(6), 599-606.
March, A., & McCormack, D. (2009). Nursing Theory-Directed Healthcare: Modifying Kolcaba’s Comfort Theory as an Institution-Wide Approach.. Holistic Nursing Practice, 23(2); 75-80.
Morse, J., Bottorff, J. L., & Hutchinson, S. (1994). The phenomenology of comfort. Journal of Advanced Nursing, 20, 189-195.
Pope, D. (1995). Music, noise, and the human voice in the nurse-patient environment. Journal of of Nursing Scholarship, 27(4), 291-296.
Walker, A. (2002). Safety and comfort work of nurses glimpsed through patient narratives. International Journal of Nursing Practice, 8, 42-48.
Wang, H., & Keck, J. (2004). Foot and hand massage as an intervention for postoperative pain. Pain Management Nursing, 5(2), 59-65.
