Introduction
The human body is a complex structure that runs on various processes, which are similar to machines. The different body parts play significant roles in the normal operation of the entire being. In order to ensure that each part runs efficiently and effectively, special care is necessary. Such care often involves special dietary requirements for the nutrition of each part of the body, exercise to ensure that most body parts remain healthy, and medical checkups as a troubleshooting mechanism for establishing what the body needs when its performance is lower than normal. This paper looks at the thyroid, a part of the endocrine system, and some of its functions. Of specific importance is the application of iodine in the thyroid gland with regard to two hormones, triiodothyronine (T3) and thyroxine or tetraiodothyronine (T4). The paper discusses the importance of the two hormones in the body, their secretion, synthesis, and distribution in the body. The paper also discusses some of the problems that the body may develop in case of lack of enough iodine in the body and the subsequent malfunctioning of the two hormones and how such problems attain resolution.
The thyroid
The thyroid is one of the largest glands in the endocrine system. The most significant functions of the gland include energy regulation in the body, protein synthesis, and control of the body’s sensitivity to hormones. The thyroid performs these tasks through the release of hormones into the body when and as necessary, with the major two being triiodothyronine (T3) and tetraiodothyronine (T4). However, the gland also produces calcitonin, which is a hormone that regulates calcium levels in the body by stimulating the movement of calcium in bones (Kovacs and Ojeda 65).
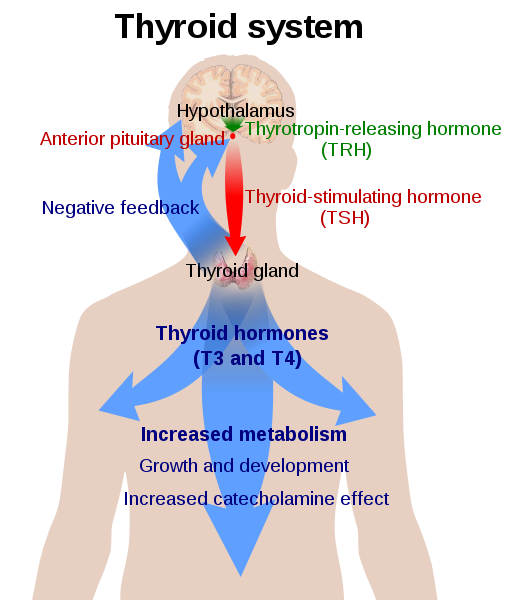
The thyroid system operates on a negative feedback system, which means that the gland is essentially active when there is a malfunction in some of the body’s operations. The feedback system consists of two other major parts namely the hypothalamus, which is located just above the brain stem and is responsible for connection between the nervous system and the endocrine system through the pituitary gland, and the pituitary gland, which located at the bottom of the hypothalamus and responsible for homeostasis. Homeostasis is the regulation and maintenance of a stable and regular internal environment in the body including aspects such as temperature (Ferreira et al. 70).
The thyroid gland performs most of its functions by releasing the relevant hormones. Although the gland is responsible for the release of nine hormones, the two major hormones and the focus of this paper are triiodothyronine (T3) and tetraiodothyronine (T4) (Ferreira et al. 70). The two hormones essentially perform the same tasks, with the main difference being their strength in performing the tasks. T3 is up to four times more powerful than T4 and thus the most organs convert T4 to T3 in the application of their metabolic functions.
Anatomy of the gland
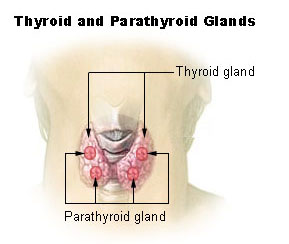
The thyroid gland or Glandula thyreoidae is located on the front side of the neck. It has a butterfly shape with two lobes in the shape of cones that go around the larynx and the trachea, which is better known as the voice box and the windpipe respectively. The gland starts just below the laryngeal prominence (Adam’s apple) and extends downwards to the fifth or sixth tracheal ring. However, it is difficult to tell the exact tracheal ring where the gland ends as it moves position during swallowing. A protective fibrous sheath, the capsula glandulae thyroidae, covers the gland in addition to the sternomastoid muscle that covers the front side. The gland is also fixed to the corcoid cartilage and the tracheal cartilage on the posterior side. The corcoid cartilage is a complete ring of cartilage that goes round the entire circumference of the trachea. The structure of the thyroid gland also consists of two parathyroid glands on each side of the cone-shaped lobes. The glands secrete calcitonin, a hormone responsible for calcium regulation in bones. The two lobes join at the thyroid isthmus, which can sometimes change in shape and size, sometimes circling the remnants of the thyroglossal duct (Brent 46).
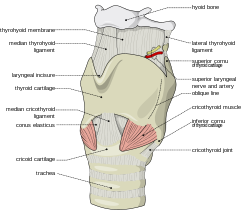
The thyroid gland starts forming in the oropharynx in a fetus and gradually makes its way down the tongue, hyoid bone, and neck muscles to its final position in the neck just below the laryngeal prominence. The connection between the original position and the final position of the gland is the thyroglossal duct, which disintegrates during an individual’s development and maturity. However, sometimes the duct remains intact, thus causing complications such as the formation of cysts that can sometimes turn cancerous. A completely developed thyroid gland weighs up to sixty grams in adults and can get slightly larger during pregnancy (Kovacs and Ojeda 83). The superior thyroid artery and inferior thyroid artery supply the gland with blood while deoxygenated blood from the gland drains through the superior and inferior thyroid veins into the jugular and brachial cephalic veins respectively.
The production of T3 and T4 hormones reach clinically significant levels twenty weeks into the gestation of a fetus although the T3 levels remain low until the fetus is at least thirty weeks old. This scenario occurs mainly because the mother supplies some of the hormones that the fetus requires during its development in the womb as the fetus’ body develops and reaches the point where it can sufficiently produce its own.
Importance of iodine
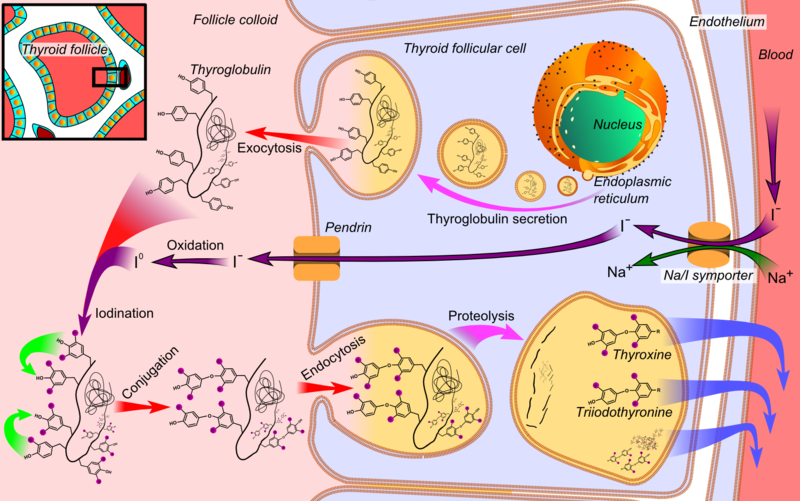
The main purpose for iodine in the gland is the creation of thyroid hormones that help in the metabolic functions of the body. Iodine plays a key role in the development of brain function and other integral body functions such as the regulation of energy, temperature, and PH levels. The main way through which iodine enters the body is by ingestion in food and fluids (Visser et al. 55). Although it gets into the blood stream, the body does not directly utilize it. Follicles in the gland absorb the iodine for the creation of T3 and T4 and store some of it in thyroglobulin, which is a diametric protein in the gland. Thyrocrytes are the thyroid epithelial cells that produce thyroglobulin. When stimulation of the thyroid occurs, T3 and T4 hormones disperse to the areas of application through carrier protein called thyroxin-binding globulin (Kohrle 180). Upon transport of the hormones to the designated destinations, the organs in need process the hormones by accessing the iodine and releasing iodine atoms that provide energy for metabolic functions.
Insufficient amounts of iodine in the body thus leaves the body indirectly prone to disorders due to insufficient creation of thyroid hormones that regulate metabolism in the entire body including critical functions such as regulation of heart rate and brain development (Venturi 156). Pregnant women are especially prone to such disorders, thus endangering the development of organs in the fetus. It is thus especially important for such individuals to ensure that their iodine levels remain optimum as too much of the mineral also causes disorders such as hypothyroidism.
Thyroid hormone regulation process
The negative feedback process involving the thyroid gland begins in the hypothalamus and ends in the various body organs that apply the hormones. When the body senses low levels of thyroid hormones in its organs, it sends signals to the brain. The hypothalamus interprets the signals and releases thyroid regulating hormones (TRH) through a tube to the pituitary gland. The hormones stimulate the pituitary gland to produce thyroid-stimulating hormones that disperse to the thyroid, thus causing the subsequent production of thyroid hormones. The thyroid glands’ follicular cells synthesize T4 from tyrosine, which is a proteinogenic amino acid on tyrosine residue of thyroglobulin (TG). The thyroid peroxidase enzyme generates hydrogen peroxide, which captures iodine from blood (Malik and Hodgson 560). The enzyme links to the benzene ring of the tyrosine residue on thyroglobulin. Upon stimulation by the TSH, the follicular cells reabsorb TG and split iodinated tyrosine from the TG. The cells form T4 and T3 and release them into the blood. In the blood, the two hormones are partially bound to thyroxine-binding globulin, albumin, and transthyretin, which are all forms of protein. The hormones cross cell membranes in the organs and bind to intracellular receptors. Although the thyroid produces both hormones, the production of the T4 hormones happens at larger quantities than the T3 due to the potency of the latter hormones in the body’s organs and the fact that the organs have the ability to transform it to T3 through the application of deiodinase enzymes (Kester et al. 3119).
Upon production, the T3 and T4hormones attach to protein receptors in the blood and travel to their organs of destination where they undergo further synthesis resulting in the release and application of iodine atoms. The resultant effect is an increase of metabolism in the organs. Most thyroid hormones in the blood go to the liver while the rest undergo synthesis in other organs including the spleen and kidney (Patrick 121). The liver is one of the most essential organs of the human body as it performs functions such as production of certain proteins for blood plasma, which aid in the transportation of iodine and other nutrients throughout the body. It also produces bile, a chemical component that breaks down fats in small intestines and clears blood of drugs and other poisonous substances. The liver removes bacteria from the blood stream and raises the body’s immunity by producing immune factors. The removal of bacteria from the blood stream is a characteristic especially attributable to iodine as one of its functions. Therefore, inactivity by the thyroid gland has negative implications on the body’s general health, which highlights further the importance of the gland’s activity in the body in relation to iodine synthesis and production of thyroid hormones.
When the thyroid hormone levels in the body organs are high, the hypothalamus stops the production of thyroid stimulating hormones. This aspect in turn halts the production of thyroid stimulating hormones by the pituitary glands and the production of T3 and T4 by the thyroid gland. In essence, the hypothalamus indirectly reduces the level of iodine in blood, hence regulating metabolic activity in the body. For instance, an increase in the levels of iodine in the body leads to an increase in the production of thyroid hormones, which increases the body’s metabolic rate leading to disorders such as fatigue, increased heart rates, and eventual cardiac problems such as heart attacks (Kovacs and Ojeda 62).
Diseases and disorders
As with most other organs in the body, the thyroid gland requires a certain amount of care, failure of which can cause dysfunctions leading to disorders and in extreme cases diseases. Therefore, every individual should ensure that the organ receives nutritional and other requirements for efficient and effective performance. There are two major dysfunctions in relation to the gland, viz. hypothyroidism and hyperthyroidism.
Hypothyroidism
This disorder is the resultant state of a body in which the thyroid gland produces fewer thyroid hormones than the body requires. Although the main cause of the dysfunction is iodine deficiency, a faulty thyroid gland or iodine-131 treatment can also cause or contribute to hypothyroidism. Individuals prone to the condition include pregnant women and individuals from both genders above the age of fifty years. Diagnosis of the condition involves testing thyroxine levels in blood whereby high levels of TSH and low T4 hormones indicate the presence of the condition. Classification of the condition into various categories mainly involves identification of the dysfunctional organ in relation to the negative feedback system. Primary hypothyroidism occurs in the thyroid gland while secondary and tertiary hypothyroidism occurs in the pituitary gland and hypothalamus respectively (Brent 40).
Signs and symptoms of this condition include weight gain, rapid thoughts, mood instability, itchy skin, fatigue, and cold tolerance among others. These symptoms may vary in different individuals and in different circumstances. These symptoms are common in disorders and diseases that result from the condition. Treatment of the condition mainly involves administration of T4 hormones into the body to cater for the deficient. Such administration occurs in tablet form, even for infants, because liquid dosage is not very accurate. Some of the conditions that result from hypothyroidism include cretinism, goiter, Hashimoto’s thyroiditis, graves disease and in extreme cases thyroid cancer.
Cretinism
Cretinism is one of the conditions that result from hypothyroidism. The condition results in stunted physical growth and slow or abnormally stunted mental growth. The disease is congenital, meaning that it is usually present before or at the time of birth, thus signifying that its occurrence and development is dependent on a woman’s care for the pregnancy throughout the entire gestation period. The most common cause of the disorder is iodine deficiency in the fetus as a direct result of inability to synthesize its own thyroid hormones and absence of sufficient thyroid hormones in the woman’s blood due to low iodine intake. When a woman is pregnant, her thyroid gland needs to produce enough thyroid hormones to cater for both her metabolic needs and those of her fetus. In cases where the woman’s dietary intake of iodine is insufficient for the production of T3 and T4hormones, the hormones that her own thyroid gland produces apply in the regulation of her metabolic processes, hence leaving little for metabolic use by the fetus. Since the fetus cannot produce clinically significant levels of thyroxine (T4) until it is at least twenty weeks old, it relies on the little T4 in its mother‘s blood resulting to insufficient T3 synthesis for application by the brain and body for required developmental purposes (Kester et al. 3121). Cases of Cretinism are lower in developed countries in comparison to developing countries as it is the norm in developed countries to execute newborn screening for low T4 levels thus providing adequate care for the condition as soon as possible. In developing countries, the case is different as lack of adequate healthcare facilities to cater for increasing populations causes a strain in the system, thus leading to the need to prioritize between several crucial healthcare procedures. Lifestyle choices also contribute to iodine deficiency as most people opt for manufactured foods as opposed to personal preparation of meals, hence losing supervisory opinions on the amounts of iodine in the food preparation process.
The clinical response to the condition in infants is the administration of artificial T4 hormones through ingestion in breast milk and formula in babies and in the form of tablets as individual progresses towards maturity.
Goiter
Goiter or a Struma is a term that applies in reference to the description of a swelling that occurs on the thyroid gland and in some cases the larynx, hence causing subsequent swelling of the neck in a bid to accommodate the inflamed organ. The description and classification of goiter mainly depends on its size and growth pattern. Referral using terms such as ‘diffuse’ is also possible depending on the pattern of the gland’s growth. Although the main cause of goiter formation is iodine deficiency, other causes include Hashimoto’s thyroiditis and Grave’s disease (Babademez et al. 1808).
Iodine deficiency causes goiter by causing stimulation of the thyroid gland and its expansion in a bid to enable it to synthesize more T3 and T4 hormones for metabolic functions. When thyroid hormone levels are low in the body, the pituitary gland senses the deficiency and releases thyroid-stimulating hormones to the thyroid gland. The thyroid expands in size to cater for the production of additional hormones that the body requires, hence leading to the visible swelling that is a goiter. Goiters are more prevalent in areas where the soil composition lacks in iodine such as mountainous regions of the Swiss Alps and areas where iodized salt is not readily available to consumers. It is less prevalent in areas where the staple food is seafood as it is naturally rich in iodine.
In areas where iodine deficiency is not a major problem, such as the United States, Hashimoto’s thyroiditis is the main cause of goiters. The disease is an autoimmune condition whereby the body’s immune system gradually destroys the thyroid, thus reducing its ability to produce thyroid hormones. Just as is the case with hormone deficiency due to iodine deficiency, the pituitary gland senses low levels of T3 and thyroxine in the body and secretes TSH, hence triggering the production of additional thyroid hormones and expansion of the thyroid to accommodate the change.
Grave’s disease
Grave’s disease is one of the conditions that occur because of hyperthyroidism, which is increased activity of the thyroid, thus causing excessive production of thyroid hormones. The disease also causes goiter by inhibiting the release of TSH through secretion of anti bodies while stimulating excessive production of thyroid hormones and the enlargement of the thyroid. Another significant effect of the condition is increased metabolic reactions leading to symptoms such as increased heartbeat, muscle weakness, insomnia, heat intolerance, and puffy skin. All these systems indicate hyperactivity in body organs thus causing the body to wear out. A significant indication of the presence of the disease in an individual is bulging eyes or exophthalmos. Although it is not always present in individuals suffering from the disease, the symptom is a certain indicator of the disease. Causes of the disorder are not certain although a majority of the cases indicate the presence of genetic factors. In consideration of the fact that the disease affects the entire function of the thyroid and the gland regulates calcium in bones though the calcitonin hormone, the disease also affects bone strength and formation. This aspect indicates that some of its symptoms may also include lack of function in body parts such as arms and legs.
Diagnosis of the condition usually involves testing TSH levels in the blood measuring free unbound T3 and T4 hormones, as the free hormones bear most of the impact on body organs, as they do not require processing. Treatment of the disease includes use of radioactive iodine that counteracts effects of excess Thyroid hormones.
Conclusion
Although the thyroid and other organs that participate in its negative feedback mechanism are small, their relevance in the body is utterly dire. The thyroid’s ability to regulate metabolic functions in the body and influence numerous other organs in the body makes the maintenance of its proper functions critical for any individual. Intake of sufficient iodine levels is one of the ways that a person ensures the proper health of the thyroid, a lack of which can lead to the development of several disorders and diseases, as mentioned in the paper. Therefore, every human being should ensure proper dietary intake of the mineral, usually through ingestion in food, water, salt, and sometimes through supplements, as is the case with infants born with Cretinism.
References
Babademez, Mehemet, Sayed Tuncay, Mohamed Zaim, Baysal Acar, Rayees Karaşen. “Hashimoto Thyroiditis and thyroid gland anomalies.” Journal of Cranialfacial Surgery 21.6 (2010): 1807-9. Print.
Brent, Gregory. Thyroid Function Testing, New York: Springer Publishing, 2010. Print.
Ferreira, Andrea, Livian Lima, Renata Araujo, Glaucia Müller, Renata Rocha, Doris Rosenthal, and Denise Carvalho. “Rapid regulation of thyroid sodium–iodide symporter activity by thyrotrophin and iodine.” Journal of Endocrinology 184.1 (2005): 69-76. Print.
Kester, Monique, Raquek Martinez de Mena, Maria Obregon, Danijela Marinkovic, Allan Howatson, Theo Visser, Robert Hume, Andgabriella De Escobar. “Iodothyronine levels in the human developing brain: major regulatory roles of iodothyronine deiodinases in different areas.” The Journal of Clinical Endocrinology & Metabolism 89.7 (2004): 3117-3128. Print.
Kohrle, Josef. “Thyroid hormone transporters in health and disease: advances in thyroid hormone deiodination.” Best Practice & Research Clinical Endocrinology & Metabolism 21.2 (2007): 173-191. Print.
Kovacs, William, and Sergio Ojeda. Textbook of Endocrine Physiology, New Jersey: Oxford UP, 2011. Print.
Malik, Raza, and Humphrey Hodgson. “The relationship between the thyroid gland and the liver.” QJM: Monthly Journal of the Association of Physicians 95.9 (2002): 559-569. Print.
Patrick, Lyn. “Iodine: deficiency and therapeutic considerations.” Alternative Medicine Reviews 13.2 (2008): 116-27. Print.
Venturi, Sebastiano. “Evolutionary significance of iodine.” Current Chemical Biology 5.1 (2011): 155-162. Print.
Visser, Edward, Edith Friesema, Jurgen Jansen, Theo Visser. “Thyroid hormone transport in and out of cells.” Trends in Endocrinology and Metabolism 19.2 (2007): 50-56. Print.
