Abstract
Cardiac arrest poses a significant threat to patients in intensive care units (ICU) and can subsequently lead to a patient’s demise. It was noted at the project site that capnography was not being used during cardiopulmonary resuscitation (CPR) despite recommendations and guidelines that supported its use in improving patient survival rates. The purpose of this quantitative, quasi-experimental project was to determine if the implementation the American Heart Association’s (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care would impact nurses’ knowledge of capnography and impact the rate of return of spontaneous circulation (ROSC) among ICU patients experiencing cardiac arrest in a hospital in New Jersey over four weeks. Tanner’s model of clinical judgement and Lewin’s change theory guided this project. Nurses’ knowledge (n = 13) of capnography was measured by the Nurses’ Knowledge of Capnography Test (NKCT). Results of NKCT revealed a statistically significant improvement from pre (M = 67.4, SD = 5.8) to post (M = 92.1, SD = 6.2), t(12) = -10.65, p =.000. Data on ROSC were obtained from facility records on 22 patients. The ROSC rate in the comparative group (n = 12) was 25% and in the implementation group (n = 10) it was 20%. A Fisher’s exact test showed a non-significant difference p =.999. Therefore, NKCT scores improved, but ROSC rate declined suggesting a clinically significant impact of the intervention on knowledge. Recommendations include continuation of the project in efforts to yield statistical significance.
Introduction to the Project
Nurses’ knowledge pertaining to clinical devices, such as capnography, used for monitoring, assessing, and treating patients with heart conditions is an important factor for achieving quality patient care and organizational effectiveness (Cook & Harrop-Griffiths, 2019). Studies conducted by Linet al. (2017), Novais and Moreira (2015), and Pantazopoulos et al. (2015) alluded to the lack of nurses’ knowledge in using capnography as recommended by the Advanced Cardiac Life Support (ACLS) to capture pertinent information about a patient’s end-tidal carbon dioxide (ETCO2) condition. They found that such low awareness of this approach presents uncertainties and poor clinical monitoring practices. Low-quality nursing practices are exemplified by the lack of awareness in using capnography when success in patient care is dependent upon the practice knowledge and use of innovative devices, such as capnography, in a clinical setting (Hamrick et al., 2017).
Similarly, Hamrick et al. (2017), Heradstveit and Heltne (2014), and Kodali and Urman (2014) linked the importance of using capnography in monitoring and gathering patient information during cardiopulmonary resuscitation events to the critical role of nursing practitioners and the knowledge of using capnography to improve patient quality care. The scholarly debate persists regarding the complexities in instituting clinical monitoring devices in the clinical setting and the lack of knowledge to effectively use the device. The rationale for this direct practice improvement (DPI) project lies in its potential beneficial effects on increasing the use of capnography in the intensive care unit (ICU) setting.
Chapter one contains critical information about this project and the selected practice problem. This is accomplished by elaborating on the background of the project, its purpose, significance, and explanation into the research problems in determining the appropriate clinical questions. The chapter also presents an overview of information regarding project design, such as methodology, design, assumptions, limitations, and delimitations. It ends by stating the organization of the remainder of the project.
Background of the Project
Cardiac arrest poses a significant threat to patients in intensive care units and is a significant factor that can lead to a patient’s demise if not addressed in a timely manner (Hartmann, Farris, Di Gennaro, & Roberts, 2015). As a result, the use of capnography to improve the outcomes of patients during cardiac arrests has been widely studied in the literature (Edelsonet al., 2014; Mader, Coute, Kellogg, & Harris, 2014). According to Cereceda-Sánchez and Molina-Mula (2017), capnography has been developed as a measurement for monitoring coronary perfusion pressure (CPP) and coronary blood flow. Recent studies have shown the effectiveness of capnography in patients’ treatment with chronic hypercapnic respiratory failure, hypoventilation, severe hypothermia, and metabolic changes clinical (Darocha et al., 2017; Cereceda-Sánchez & Molina-Mula, 2017; Chhajed et al., 2016). However, Leppink, O’Sullivan, and Winston (2016) noted that despite the existence and widespread use of capnography in practice improvement, many nurses still show some levels of uncertainty due to the reduced awareness in the knowledge and application of capnography in clinical settings.
Recent studies conducted by Dioso (2014) and Duckworth (2017) amplified the importance of equipping nurses with the knowledge of the application of capnography as a technique to manage cardiac arrest incidence among patients. It has been noted in the research that these training approaches should address knowledge barriers about capnography and its applications in improving a patient’s quality of care (Israel, 2014; Jaffe, 2017; Kuisma et al., 2017; Nassar & Schmidt, 2016).
The major concern for healthcare practitioners is to minimize the negative impact created by the uncertainties and the lack of knowledge by nurses in using capnography. This relationship between nurses’ adoption of capnography, clinical uncertainty, lack of knowledge to use capnography in clinical settings, and its impact on patient care remains understudied (Kodali, 2013; Whitaker & Benson, 2016). Sandroni, De Santis, and D’Arrigo (2018) argued that the lack of knowledge among users monitoring devices, such as capnography, could result in patient fatality. The scholars also uncovered a gap in the literature pertaining to nursing practices in the use of this monitoring device to minimize medical errors in a clinical setting as well as nurses’ adoption of capnography, clinical uncertainty, and the lack of knowledge for using capnography in a clinical setting (D’Arrigo, 2018). Further investigation could expand the understanding of nurses’ role in adopting capnography and determine the levels of clinical uncertainties resulting from the lack of device monitoring knowledge in the healthcare industry (Kaminska, Wieczorek, Dabrowski, Nadolny, & Smereka, 2018).
At the project site, there was no existing policy for the use for capnography in the ICU. The project site reviewed and analyzed resuscitation data monthly, including ETCO2 monitoring which was measured by capnography. It was recognized that ETCO2 monitoring the documentation was incomplete and or not recorded on the Code Blue sheet. The intent of this project was to incorporate ETCO2 monitoring into the cardiopulmonary resuscitation policy to utilize during every Code Blue. All code carts were equipped with capnography monitoring devices for measuring and the documentation that was recorded on the Code Blue sheet. Monitoring ETCO2 has been recommended to confirm proper endotracheal tube placement, to assess efficiency of chest compressions, and to gauge return of spontaneous circulation (Panchal et al., 2019)
Problem Statement
The American Heart Association’s (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care (Panchal et al., 2019) recommended the use of capnography for measuring ETCO2 to assess and measure return of spontaneous circulation (ROSC). It was not known if or to what degree the implementation of the American Heart Association’s (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Emergency Care would impact nurses’ knowledge of capnography and increase the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest when compared to current practice in urban New Jersey. Previous studies conducted by Hassankhani, Aghdam, Rahmani, and Mohammadpoorfard, (2015) and Kiekkas, Stefanopoulos, Konstantinou, Bakalis, and Aretha (2016) showed that nursing practice pertaining to the application of evidence-based technology, such as capnography, is essential for managing cardiac-related incidents. In addition, the perception exists that if nurses possess sufficient knowledge pertaining to the use of capnography during cardiopulmonary resuscitation (CPR), they can achieve better outcomes for the patient, especially in monitoring patients’ heart conditions and reducing risks of complications during a direct peritoneal resuscitation (DPR) (Hassankhani et al., 2015). According to the literature, nurses have a lack of knowledge about how to use new innovations such as capnography (Mohamed, 2019; Saunders, Struya, Pollock, Mestek, & Lightdale, 2017; Wright, 2017). Specifically, at the project site, there is an inconsistent use of capnography. This presents a need for an improvement in practice to maintain patient safety. Capnography will help to improve care and increase patients’ safety.
Purpose of the Project
The purpose of this quantitative, quasi-experimental project was to determine if and to what degree the implementation of the AHA Guidelines for Cardiopulmonary Resuscitation would impact nurses’ knowledge of capnography and the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest when compared to current practice at a 20-bed ICU in an acute care hospital in Southern New Jersey over four weeks. The independent variable identified in this project was the intervention program designed to improve nurses’ knowledge of capnography use. The two dependent variables were nurses’ knowledge of capnography, which was measured by the Nurses’ Knowledge of Capnography Test (NKCT), and the rate of return of spontaneous circulation (ROSC), which was obtained from the unit’s Code Blue sheet. The nurses practicing in Southern New Jersey at the project site facility implemented this quality improvement project. The selected group of staff participants was appropriate for the project because of their clinical exposure to the use of capnography.
This project was focused on ascertaining the strength, vulnerabilities, and weaknesses specific to nurses’ awareness about the use of capnography during cardiopulmonary resuscitation. Additionally, the project examined the correlation between such knowledge and the use of capnography during CPR and determined if any correlations existed between nursing knowledge and patient outcomes related to ROSC rates.
In addition to addressing the research deficit on this topic as well as providing the necessary insight for clinical managers, this project also attempted to provide some understanding of the differences in the nursing knowledge in using capnography during cardiopulmonary resuscitation. Moreover, it offered new information to achieve efficiency in the adoption of capnography in managing patients with CPR. The outcomes of this project included a positive clinical nursing practice change in which clinical managers used the results of the initiative to moderate nurses’ adoption of clinical devices in the hospital setting.
Clinical Questions
The use of capnography by nurses is a strategic approach to achieving positive clinical outcomes (Panchal et al., 2016). According to previous studies, the lack of knowledge and the inability of nurses to adopt innovation, such as capnography, can result in unintended consequences such as clinical uncertainties, medical error, and even patient fatality in a clinical setting. The clinical questions that guided this DPI project were:
- Q1: Does the implementation of the AHA Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care impact nurses’ knowledge of capnography, compared to current practice, among ICU nurses in an acute care hospital in Southern New Jersey over four weeks?
- Q2: Does the implementation of the American Heart Association’s Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care for Emergency Care impact the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest in an acute care hospital in Southern New Jersey over four weeks?
Although this quality improvement projects helped to increase awareness, the risk of developing negative patient outcomes was a concern. The clinical questions related to the problem statement by addressing patient outcomes related to cardiac, pulmonary resuscitation, and the ROSC in the ICU setting. Although the AHA’s Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care recommended using capnography to evaluate ROSC’s return, it has been underutilized in acute care settings. Capnography applications can provide valuable input in monitoring ETCO2 levels during resuscitation. According to the AHA, a sudden and sustained increase in ETCO2 to normal value during cardiopulmonary resuscitation is a strong ROSC indicator (Panchal et al., 2019). By recognizing ROSC before checking for a pulse, interruption in chest compressions can be minimized; therefore, the patients’ chance of survival increases during CPR.
The clinical questions consider three variables. The independent variable under consideration in both questions was the intervention program for improving nurses’ knowledge of capnography use based on the AHA’s Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. The dependent variable for the first clinical question, then, was nurses’ knowledge of capnography, which was measured by the Nurses’ Knowledge of Capnography Test (NKCT) (Kiekkas et al., 2016). The dependent variable for the second clinical question was ROSC, which was obtained from the facility Code Blue datasheet, specifically for the documentation of end-tidal CO2 monitoring during CPR.
Advancing Scientific Knowledge
The outcomes of the DPI project could contribute to the development of population health outcomes for patients suffering from cardiovascular diseases. This was accomplished by the provision of clinical practice evidence resulting from this project and its effect on coronary care. The findings in the proposed quantitative quasi-experimental project could be used by clinical managers to moderate nursing practices in the adoption of new clinical devices such as capnography. Edelson et al. (2014) estimated that over 200,000 people suffer cardiac arrest annually, and more than 80% of them do not survive to discharge (p. 353). Kodali and Urman (2014) and Mader et al. (2014) found that thousands of people die from cardiac arrest in the United States every day. Thus, cardiac arrest is a common problem that affects various demographic populations in the United States, demonstrating the relevance and importance of this DPI project to current medical science.
Studies by Kiekkas (2016) and Lui, Poon, and Tsui (2016) advanced the knowledge for the use of capnography in the clinical setting to monitor and improve survival rates of cardiac-related incidents. However, the research outcomes surrounding the cases in which nurses lack the knowledge to use capnography have proven to be inconsistent, thus creating difficulties and uncertainties for targeted practice improvement measures (Dioso, 2014). To improve capnography practices in clinical settings, nurses and clinical managers must understand the relationship and importance of using capnography to improve patient outcomes. This project closed the gap in the information about nurses’ adoption of capnography, clinical uncertainty, and the lack of knowledge to use capnography in a clinical setting. It also contributed to the larger body of literature and application to nursing practices.
The theoretical foundations for the study were based on the model of change introduced by Kurt Lewin in the 1940s and Tanner’s model of clinical judgment published in 2006. Lewin’s theory proposes that all change projects happen in three steps: unfreezing, moving, and refreezing (Lewin, 1951). Lewin (2003) noted that each stage is invaluable, meaning that they all play a role in the new structure or objective becoming a part of the existing system. This theory implies that people are resistant to change, especially if they do not understand why it is necessary (Burnes & Bargal, 2017). Moreover, the process of a change’s introduction can be influenced by using the elements outlined in the “unfreeze” step.
Lewin’s (1952) view of change projects provides a helpful framework for understanding and explaining the processes and ideas relating to the adoption of new techniques, applications, and systems in a variety of organizational settings such as health care centers. In the case of nursing knowledge and capnography, this theory was used to demonstrate that the complexity of an innovation and its compatibility with an existing system were crucial in the success of its implementation. Thus, the project, which targeted nurses’ knowledge and training, used this approach to measure the correlation between knowledge and use of the procedure and provide insight into nurses’ changing attitudes towards capnography in CPR.
Christine A. Tanner (2006) outlined four phases of nurses’ clinical decision-making, highlighting that nurses’ knowledge and the unit’s culture can affect clinical judgments. According to Tanner, the term “clinical judgment” describes the process of thinking and reasoning, during which the healthcare provider uses objective and subjective data about the patient and arrives at a conclusion about one’s treatment. The four phases reflect the steps that a nurse should take when making a decision, including preparation to address the problem and actions to perform when the decision has been implemented.
The first phase of a nurse making clinical judgment is noticing. It describes how nurses compare the expectations of the patient’s clinical situation to the results of their assessment. After nurses identify the most important data, they enter the second phase, interpreting. Tanner (2006) stated that nurses should utilize specific reasoning patterns (analytic, intuitive, or narrative) to compare data and separate information. The analyzed data is used in the next step – responding. Nurses act according to their decisions, act, or monitor the patients. Lastly, nurse engage in reflecting; reflection has to occur when during and after the patient’s treatment to evaluate potential incorrect choices and improve critical thinking.
Tanner’s model of clinical judgment was relevant to the present project because it highlights the role of knowledge in nurses’ clinical judgments. In her seminal work, Tanner (2006) argued that clinical judgments are strongly impacted by the culture in the nursing unit and the context of every practice-related situation. Thus, the learning intervention introduced in the DNP project had the potential to change the environment of the unit and lead to improved clinical decisions in the use of capnography during resuscitation.
Tanner’s ideas aligned with the project’s proposal that nursing education in a topic, such as capnography, can impact their decision-making and inform clinical judgments before and during CPR. As she suggested, the four phases are what makes each clinical decision well thought-out. Teaching nurses about capnography and its benefits may have influenced the nurse participants’ interpreting and responding phases. For instance, a nurse considering a response to a patient with cardiac arrest and equipped with specific knowledge can choose to use capnography during resuscitation, believing that it will lead to better outcomes.
Significance of the Project
A gap existed in the literature about whether increased nurses’ knowledge of capnography was associated with the increased use of capnography during CPR (Kodali, 2013; Whitaker & Benson, 2016). The significance of the project lay primarily in addressing the inconsistent findings in the scholarly literature on capnography and nurses’ knowledge regarding its use during CPR in the ICU. Current literature on capnography focused primarily on the outcomes and implementation of capnography within this healthcare setting (Kalmar et al., 2018; Langhan, Shabanova, Li, Bernstein, & Shapiro, 2015; Turle, Sherren, Nicholson, Callaghan, & Shepherd, 2015). To facilitate the effective use of capnography, determining which individual factors impacted nurses’ knowledge and the understanding behind the readiness to use capnography in practice was essential.
This project aimed to explore the link between nurses’ knowledge and the use of capnography during CPR, thus providing the basis for further practice improvement and scholarly work in this area. The results of this initiative could have also led to the improvement of practice approaches in capnography and an enhancement in the quality of patient outcomes in the intensive care unit setting. This project differed from other studies in the field of capnography use in terms of its focus; however, it also built on other research concerning the nurses’ perspectives on capnography and its importance in promoting successful patient outcomes (Lin et al., 2017; Novais &Moreira, 2015; Pantazopoulos et al., 2015).
Furthermore, the project filled in the gaps in the literature by correlating the data provided by quantitative studies of capnography and the nurses’ knowledge of the topic as well as its application within the present intensive care unit setting. As such, the results of this project are critical for a variety of stakeholders, including nurses, managers, patients, and the industry. The results of the data collected during this project’s duration rely on practice improvements in education and training. The outcomes of the intervention contributed to population health by enhancing clinical practices in CPR and the improvement of capnography efforts within this setting. Also, the educational program had the potential for decreasing uncertainty during resuscitation procedures and practices that could stem from a lack of nurses’ knowledge, reducing stress, and promoting guideline compliance within the ICU. Overall, the project provided valuable information in support of nursing education and training in capnography, which helped to advance the practice and improve population health.
Rationale for Methodology
The quantitative method was chosen for this project as it relies on numerical data. The measures in this project were numerical: capnography use as measured by nurses’ data input in the electronic health record (EHR) and nurses’ knowledge as measured by the NKCT (see Appendix B). In the quantitative methodology, data gathering is the primary strategy for getting information from project participants (Kiekkas et al., 2016). The quantitative method was considered most appropriate for this project because the relationships between individual factors affecting capnography use and nurses’ knowledge during CPR practice in ICUs were examined.
Quantitative methodologies have many benefits that are relevant to this project. They provide a high level of validity and certainty of results as they apply statistical tools for data gathering, organization, and analysis (Ali & Bhaskar, 2016; Center for Innovation in Research and Teaching [CIRT], 2013a; Heale & Twycross, 2015; Leppink et al., 2016; Watson, 2015). The use of the quantitative method in this project was strategic in answering the clinical questions to clarify the relationship between the independent and dependent variables (Campbell, 2017; CIRT, 2013b; Guo et al., 2016; Nelson, 2018).
A qualitative methodology was not be used in this project because it contains some limitations that could possibly influence and hinder the reliability of data findings. Qualitative methods are concerned with abstract concepts, and thus their ability to provide objective information is limited (Flick, 2018; Green & Thorogood, 2018). The focus of qualitative methods is on understanding participants’ behaviors and attitudes rather than specific activities or knowledge levels, which can affect the results of the data (Austin & Sutton, 2014; Barnham, 2015; Flanagan, Greenfield, Coad, & Neilson, 2015; Gunnell, 2016). In addition, qualitative instruments are usually not checked for validity and reliability, which increases the risk of bias. Moreover, qualitative studies allow for subjective collection and analysis of data in which the researcher is also a participant in the study (Katz-Buonincontro & Anderson, 2018; Rowley, 2014).
A qualitative method would have contradicted the purpose of the project and affected the opportunity to use the results for practice improvement. As such, a quantitative study was determined to be more effective for answering the clinical questions. The central question posed for the project considered the participants’ level of knowledge and its connection to the use of capnography. By addressing the chosen question with quasi-experimental analysis, not only did the data provide the answers to address the gaps in the project’s design, but it also addressed the questions about whether improvements in nursing knowledge in the use of capnography had any significance in influencing its use within an ICU.
Nature of the Project Design
A quasi-experimental design was selected for this project because it contains specific procedures that aligned with the project purpose and clinical questions. The focus of the project was on assessing the effect of the independent variable on the dependent variables. The quasi-experimental design is similar to an experimental one in that it analyzes the connection between independent and dependent variables (Watson, 2015). The primary difference between the two designs is that a quasi-experiment does not use randomly assigned subjects; instead, it relies on a thoughtfully selected sample (Watson, 2015). Thus, the first alternative to quasi-experimental design is experimental design, but this approach would have been inappropriate for this project as it would have been difficult to obtain random subjects for both practical and ethical reasons.
Moreover, some non-experimental designs exist. These strategies do not engage the independent variable; instead, they simply observe the events as they occur (Watson, 2015). For example, observational research provides a view into a subject’s behavior in a natural setting (Watson, 2015). Here, the investigator does not introduce any new interventions and does not measure changes. Cross-sectional and correlational research designs are also non-experimental – while two or more groups and variables can be compared, the investigator still does not attempt to improve or otherwise influence the participants’ actions (Watson, 2015). These approaches did not fit for the present project because they do not consider change as the basis of their methodology.
The independent variable for this project was the intervention for nurses based on the AHA Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care (Panchal et al., 2019), specifically the use of capnography during CPR. The independent variable included an educational program that trained the ICU nurses at the project site on the AHA guidelines. The first dependent variable was nurses’ knowledge of capnography as measured by the Nurses’ Knowledge of Capnography Test (see Appendix B) (Kiekkas et al., 2016). The second dependent variable was ROSC, which was obtained from the facility Code Blue datasheet, specifically for the documentation of end-tidal CO2 monitoring during CPR.
Data on the use of capnography four weeks before and four weeks after the implementation of the educational intervention were collected. They were then compared to evaluate the affect the independent variable, the AHA guidelines and related educational intervention based on AHA guidelines, had on the dependent variables, nurses’ knowledge of capnography and ROSC rates during CPR. The quasi-experimental research design relies on quantitative data collection and analysis methods to examine the relationship between two or more variables (Ingham-Broomfield, 2014). The variables used in quasi-experimental designs, such as nurses’ knowledge and ROSC, closely reflect the true experiences and perceptions of the participants in a project (Price, Jhangiani, Chiang, Leighton, & Cuttler, 2017).
There were two sample populations in this project. The first sample included all nurses working the project site ICU. During the time of the project, there were 32 nurses working in the unit. Structured questionnaires containing the selected survey instruments were used for data collection in this project. The surveys collected demographic data, including nurses’ age, race, sex, job title, and nursing experience, but excluded identifying data such as their names, medical records, and social security numbers. Nurses’ knowledge was then measured using the NKCT before and after an educational intervention PowerPoint on using end-tidal capnography monitoring during cardiac resuscitation.
The second sample were patients who received care in the ICU of a hospital in Southern New Jersey during the project time frame. The patient sample size was limited because, while the ICU is licensed for 20 beds, it was operating at limited capacity, eight to ten beds, for the duration of the project. Patient inclusion criteria were adult age (over 18 years old), admission to the unit, and in-hospital cardiac arrest with the following performance of CPR. Patient exclusion criteria were patients’ age (patients younger than 18 years old were not considered), lack of admittance to the unit, and any documents or standards that did not lead to nurses performing CPR following cardiac arrest.
The patient sample was pulled from the electronic health record (EHR) and compiled into the code committee data collection sheet by the quality committee nurse (QCN). The patient data were de-identified and given to the primary investigator. The data included the number for ETCO2 (measurement for capnography use) and ROSC that were recorded during CPR. The patient data were de-identified. Data were collected on the patients who met the inclusion criteria for four weeks before and four weeks after the implementation of the project.
Definition of Terms
This section provides a brief overview of the operational terms of the project:
- Capnograph. The instrument used to measure and display the amount of carbon dioxide (CO2) in one’s breath (Kiekkas et al., 2016).
- Capnography. Capnography is a non-invasive technique to monitor the concentration of partial pressure of CO2 (Kiekkas et al., 2016). It can aid a nurse in tracking a patient’s progress and support decision-making during CPR.
- Cardiac arrest. This term is defined as “the cessation of cardiac mechanical activity confirmed by the absence of a detectable pulse, unresponsiveness, and apnea” (Tobi & Amadasun, 2015, p. 132). Cardiac arrest leads to a patient’s death if the appropriate care is not provided immediately.
- Cardiopulmonary resuscitation (CPR). This term identifies the process of restoring the patient’s blood flow during a cardiac arrest using chest compression and artificial ventilation (Kodali & Urman, 2014). There are specific, detailed guidelines on how to perform CPR that provide the foundation on which the assessment of the nurses’ knowledge regarding this technique was based in this project.
- Electronic Health Record (EHR). An EHR is a digital version of a patient’s record that contains information about patients and is updated in real time (Lin et al., 2018). An EHR allows hospitals to collect, systematize, share, and use patient data for diagnosis and treatment.
- Nurses’ Knowledge of Capnography Test (NKCT). The NKCT is a psychometrically comprehensive instrument for evaluating nurses’ knowledge about capnography. It is recommended that the nurses’ knowledge be re-validated beyond the anesthesiology department and the NKCT be used for the assessment of educational programs on capnography (Kiekkas et al., 2016).
- Return of spontaneous circulation (ROSC). This term refers to the resumption of a normal heart rhythm (sustained perfusing cardiac activity) that occurs after cardiac arrest (Elola et al., 2019). Return of spontaneous circulation is defined by the patient having a palpable pulse, moving, breathing, or coughing. Such efforts as defibrillation and cardiopulmonary resuscitation can increase the changes of ROSC for the patient.
Assumptions, Limitations, Delimitations
The following methodological assumptions were made in this project:
- The information gathered from the participants reflected the overall situation in an ICU of a 240-bed hospital in Southern New Jersey. Although the nursing sample was small, and there may have been individual differences among the participants, it was assumed that their attitudes and perspectives would match those of nurses working within a similar setting under similar situations. It was likely that the ICU had similar standards, training, and equipment available for its medical staff as similar ICUs.
- It was assumed the nurses selected for the project would have time to participate in the testing portion of the project to obtain data to answer the first clinical question. The chosen quantitative methodology implied that each participant would complete the NKCT both pre- and post-educational intervention. This test assessed the nurses’ education and information retention on the subject and how they perceived the importance of this procedure within the clinical setting. Nurses have busy schedules, but an expectation was that their participation in the project would help them to obtain the appropriate information and improve patient outcomes as a result.
The project limitations were:
- A lack of funding prolonged the data collection process. Providing compensation to nurses for taking part in testing would have increased the response rate and nurses’ willingness to participate in the project.
- The site was a small community hospital. The sample size was limited because the ICU has 20 licensed beds but had been operating at an eight to ten bed capacity. Therefore, the project results are generalizable to other units within the site but are not generalizable to larger populations outside of the project site.
- As the COVID-19 pandemic was evolving daily and the number of cases were rising in New Jersey during the project timeframe, the availability of portable capnography equipment use in negative pressure rooms may have been limited. Additionally, appropriate staffing was a limitation as the pandemic continued, and nurses’ clinical judgment might have been be compromised due to stress and increased workload.
The proposed delimitations within this project were:
- The study’s delimitation was the site, a small community hospital located in a hospital in Southern New Jersey. With limited bed space, all the beds were not being used.
- The site only had two portable capnography monitors available, which meant that nurses will be only able to use capnography in two simultaneous Code Blue situations. If a third code occurred, then the project’s results would have been influenced. Any such instances were recorded to ensure transparency.
Summary and Organization of the Remainder of the Project
Overall, CPR is an essential process in coronary care settings, and additional techniques could increase the chances of survival. As shown above, the rates of people suffering from cardiac arrest annually are high, while the rate of survivors is low (Edelson et al., 2014). Capnography has been shown to be a valuable addition to the standard CPR procedures in monitoring the patient’s condition and predicting adverse events (Hamrick et al., 2017; Heradstveit & Heltne, 2014; Kodali & Urman, 2014; Venkatesh & Keating, 2017). The examination of the available data revealed the need to explore the barriers to the consistent implementation of capnography use and its effects at the project site in particular and in ICU settings in general. Furthermore, the previous research also demonstrated the importance of examining the nurses’ knowledge and attitudes toward capnography in CPR and their utilization of these concepts in practice (Saunders et al., 2017; Wright, 2017). Some studies suggested that many nurses are hesitant to apply such techniques due to the lack of proper training and experience (Lin et al., 2017; Lin et al., 2015; Novais & Moreira, 2015; Pantazopoulos et al., 2015).
This topic was limited in the literature, which indicated gaps in data on how nurses’ knowledge may affect their readiness to use capnography while complying with standard procedures. The project aimed to advance the knowledge in this area, and the insight gained could be useful for nurses in the improvement of patient outcomes and practice. This present DPI project sought to address this problem by establishing the relationship between nurses’ knowledge, the use of capnography, and how they correlate into contributing to positive patient outcomes.
This project advanced the research in the fields of nursing knowledge and capnography use, providing an insight into how nurses’ education could or could not translate into an improved decision-making process. As based on Tanner’s (2006) theory, nurses’ clinical choices greatly depend on the knowledge they possess and the environment in which they work. This project challenged the assumption that education would be enough to influence nurses to change by using Lewin’s change model as a framework for the intervention.
The project employed a quantitative methodology, which provided the investigation with a transparent way of data collection and analysis. The quasi-experimental design was chosen due to the ability to control variables and select a sample that corresponded to the project aim. There were three variables in the project – the independent variable was the educational intervention based on the AHA guidelines on the use of capnography during resuscitation. The dependent variables were the nurses’ knowledge about capnography and the rate of ROSC in patients who experience cardiac arrest and underwent resuscitation in the unit.
The literature review provided in Chapter Two will present an in-depth view of the barriers associated with capnography use as they relate to nurses’ knowledge through the examination of scholarly findings on the topic and its importance within the clinical setting. Chapter Three of the project will explore the selected quasi-experimental methodology for data collection and analysis. Data analysis will be documented in Chapter Four, which will also demonstrate the calculations of the study in visual form. Finally, Chapter 5 will provide a discussion of the project and its connection to the existing scholarship and practice environment.
Literature Review
At the present time, capnography is applied as a monitoring tool in a variety of clinical settings, including the operating theater and intensive care units (ICUs). Its main purpose is to help nurses assess patients’ end-tidal carbon dioxide (ETCO2) levels (Conway et al., 2018). This information allows one to understand the efficiency of a person’s metabolic and respiratory functions while under medical care. Additionally, during cardiopulmonary resuscitation (CPR), capnography provides an evaluation of both the cardiac function and organ perfusion, allowing monitoring of the effect of CPR efforts and predictions regarding the restoration of spontaneous circulation (ROSC). The purpose of this quantitative, quasi-experimental project was to determine if and to what degree the implementation of the AHA Guidelines for Cardiopulmonary Resuscitation would impact nurses’ knowledge of capnography and the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest when compared to current practice at a 20-bed ICU in an acute care hospital in Southern New Jersey over four weeks. Thus, the main themes discussed in the literature review are concerned with the use of capnography, especially when performing CPR, nursing knowledge, and patient outcomes.
The present literature review considers the information from peer-reviewed journals, conference proceeding publications, and. Academic journals were the foundation of the project’s investigation, as the recent knowledge contained in the peer-reviewed articles showed the current use of capnography as well as the aspects (weaknesses, strengths, and potential problems) of its use in the clinical sphere. The collected articles contained the analyses, debates, arguments, and discussions pertaining to contrasting and similar reviews relating to the use of capnography in a clinical setting.
This chapter will discuss the use of capnography in clinical settings, including the information on the procedures’ history, the evolution of the question posed in this project, and the potential gaps in the literature identified in the scholarship. The next section then offers a brief overview of the theoretical foundation for the project. The final section includes an extensive review of the literature.
There are four main themes explored in the literature review section. The first theme highlights capnography and alternatives in resuscitation and includes an overview of articles regarding the history of capnography in resuscitation. The second theme focuses on different uses of capnography with summary and analysis of articles regarding capnography outside of resuscitation and capnography use in resuscitation. The third theme of the literature review centers on nursing knowledge and patient outcomes with specific focus on nursing knowledge about capnography and other procedures. The fourth theme covers specific protocol for using capnography and includes resuscitation specific utilization and education for expanding utilization, and barriers related to utilization. A summary offers a discussion of how these themes connect to the project problem and purpose in addition to a discussion of how this project addresses the gaps revealed in the literature review.
These topics offer an academic, logical, and rational discussion of reviews on nurses’ use of capnography as part of clinical practice in relation to patient management during cardiopulmonary resuscitation. They include subsections that discuss alternatives to capnography, nurses’ attitudes to CPR and capnography, and the impact of change on nurses and patient outcomes.
The search for the appropriate studies involved relevant key words such as capnography, resuscitation, cardiopulmonary, resuscitation, innovation, clinical setting, and cardiac. These key words were utilized when searching through several databases, including but not limited to Elsevier, NCBI, and PubMed, and ProQuest Central. Prior to being selected, all articles were appraised according to their relevance to the project’s topic, date of publication, clinical question(s), methodology, quality of evidence, and limitations acknowledged by the investigators.
The understanding of capnography invention, its initial use, and current trends help enhance the knowledge of the implications of its application and the prospects for the future development of capnography. From a historical perspective, capnography is a relatively new approach to evaluating a patient’s health state. The introduction of capnography to the clinical setting in the United States occurred in 1978, and registered nurses began using this tool in recent years to aid patient care (Harper, 2005). However, capnography as an instrument was developed in the 20th century, indicating a long history of its use in medicine (Kalenda, 1978). Hence, one can see the early onset of the problem of the uses of capnography in medical care.
One of the main issues considered in literature is the use of capnography in emergency and non-emergency situations as well as different units of the hospital. Wright (2017) argued that although capnography has been used in the clinical setting for many years, the actual use of this approach was limited. Anesthesia procedures and the practice of using capnography instruments for monitoring cardiac attacks have gained attention in its application in the healthcare setting. Gravenstein, Jaffe, Gravenstein, and Paulus (2011) stated that capnography can be used to measure CO2 levels, metabolism, circulation, and other useful metrics, providing an extensive assessment of a patient’s well-being that is useful not only in emergency care but also in the day-to-day monitoring of patients. Therefore, capnography as a monitoring tool provides medical personnel with a better understanding of a patient’s health state because the interpretation of waveforms can serve more purposes than the measurement of ETCO2 alone.
This DPI project strengthened the argument that capnography’s uses are wide in the ICU. The following section offers a discussion of the theoretical framework for this project. Then, the literature, categorized into themes and related subthemes, is addressed.
Theoretical Foundations
The theoretical foundations of the present project were Tanner’s model of clinical judgment and Lewin’s change theory. Tanner’s model provided the framework for the practical application of the project to nurses’ workflow. At the same time, Lewin’s model provided the mode through which the change in practice was implemented at the project site.
Tanner’s model of clinical judgement. Tanner introduced her theory in 2006, posing that there are four main steps for a nurse to take to make a clinical judgment: noticing, interpreting, responding, and reflecting (Tanner, 2006). The first step, noticing, pertains to nurses comparing the expectations of the patient’s clinical situation and the results of the nursing assessment. As the nurse identifies the most critical clinical data, the next step, interpreting, begins. Here, Tanner (2006) argued that the nurse must apply reasoning patterns (analytic, intuitive, or narrative) to compare data, cluster information according to the fact’s relation, check accuracy, and distinguish accuracy, reliability, and relevance. Then, the judged data are used for complication prediction and the next step – responding. One may need to act or monitor the patient further, delegate some tasks, or choose which activities have higher priority. Finally, the nurse’s last phase is reflecting; reflection needs to happen during taking action to treat the patient as well as after the treatment to assess potential incorrect judgments and strengthen critical thinking.
Tanner’s model of clinical judgment is relevant to the present project because it highlights the role of knowledge in nurses’ clinical judgments. In her seminal work, Tanner (2006) argued that clinical judgments are strongly impacted by the culture in the nursing unit and the context of every practice-related situation. Thus, the learning intervention introduced in the DNP project had the potential to change the environment of the unit and lead to improved clinical decisions in the use of capnography during resuscitation.
Lewin’s change model. Originally introduced by Kurt Lewin in the 1940s, the change model is still used by businesses and other organizations to this day. It is an approach to change that is based on three main stages: unfreeze, change, and refreeze (Lewin, 1951). Each of these steps contains a list of specific actions that aim to lower participants’ resistance to change and increase the chance of the implemented change becoming the new standard. The first stage, unfreezing, implies that the current order of operation must be uprooted in order to introduce new objectives. Here, the change is to be viewed as necessary – the organizational beliefs can be challenged with evidence, information dissemination, planning, and refocusing (Morse, 2017). Next, the step of changing involves all processes that are needed to institute the new order in the place of the old status quo. Here, the evidence transforms into the project, and its elements are completed to create the new system. Finally, the refreezing stage ensures that people continue to embrace change and that any problems are addressed timely.
In Lewin’s (1951) seminal work, he introduced the stages and discussed the importance of them, showing how unfreezing and refreezing affect the attitude of involved persons towards change. Many contemporary researchers have analyzed the change model and showed how it is still relevant to management. Burnes (2004) and Cummings, Bridgman, and Brown (2016) considered this model one of the most valuable business and management theories ever created. The two sets of researchers noted that Lewin’s change model has roots in both psychological and business ideologies, acknowledging people’s resistance to new information and change and devising approaches that address this barrier. Hussain et al. (2018) and Burnes and Bargal (2017) showed that while the simplistic formula of three steps can be questioned, its role in innovation is valuable for all industries and spheres where employees play a significant role in the success of the system.
Lewin’s model of change was chosen as a theoretical foundation for this project due to the abundance of medical research using this approach and their results in its implementation. According to Udod and Wagner (2018), this approach has been widely used in healthcare. Its use of steps and the view of employees as vital members of the process can help nurses to adjust to the new procedure. Capnography is known among nurses, but its use can be limited due to staff’s knowledge and perception of its usefulness (Kaminska et al., 2018). The clinical questions posed in this research examined how this barrier can impact patient outcomes and how new practice can lead to positive results. Thus, as change burdened by negative perceptions lay at the core of this project, Lewin’s change model was instrumental for achieving results.
Review of the Literature
At the present time, capnography is applied as a monitoring tool in a variety of clinical settings, including the operating theater and intensive care units (ICUs). Its main purpose is to help nurses assess patients’ end-tidal carbon dioxide (ETCO2) levels (Conway et al., 2018). When patients are faced with an unexpected life-threating event, they might not have their choice of hospital to care for them in their time of need. An example of one such emergency would be a critical event such as cardiac arrest. Per emergency medical transport (EMT) guidelines the patient is transported to the nearest hospital cardiac arrest management. Cardiac arrest is a major public health concern, given that there are approximately 420,000 cases annually in the United States (Edelson et al., 2014). Per AHA guidelines, it is expected that the use of new and innovative technology, such as capnography, is the standard of care for assessing and monitoring changes in patients’ conditions (Panchal et al., 2019). Capnography should also be utilized for patients presenting with signs and symptoms of respiratory distress, intubation, and those who necessitate CPR interventions (Panchal et al., 2019). The site for this DPI project was in Southern New Jersey, a small suburban hospital ICU licensed for 20 beds but operating at an eight to ten bed capacity with a population of 87,065 persons. In this community, there were three surrounding acute care hospitals. However, patients requiring emergency care for cardiac event were transported to the nearest location, such as the project site. The intent of the project was to assess nurses’ knowledge of the use of capnography and how that impacted ROSC.
The present literature review presents information from peer-reviewed journals, conference proceedings publications, and books that informed the DPI project. The literature were collected from academic databases, including Elsevier, NCBI, PubMed, ProQuest Central, and Google Scholar, using the keywords capnography, resuscitation, cardiopulmonary resuscitation, innovation, clinical setting, and cardiac. The inclusion criteria included articles from peer-reviewed publications released between 2000 and 2020 in full-text and written in the English language. An exception from these criteria was made for seminal studies, specifically those by Lewin and Tanner. Moreover, one older study that introduced capnography for use during CPR was also added to demonstrate the history of the capnography use (Kalenda, 1978). The database searches yielded over 5,000 results, which were then checked for relevance to the topic. After inclusion and exclusion criteria were applied, 56 studies were chosen for review, including those used to discuss the background and theoretical foundations of the project.
Three main themes were identified in the literature that were relevant for this project. The first theme is the background of capnography, including the history of how capnography was implemented into the various sectors of healthcare, such as anesthesia, respiratory problems, and resuscitation. The second theme focuses on nurses’ knowledge and patient outcomes with an analysis of nurses’ knowledge about capnography, specific protocols for utilizing capnography in care, and specific guidelines for using capnography during resuscitation. The third theme of the literature review centers on nursing education about capnography that aims to widen its use with specific focus on various interventions and barriers that healthcare providers encounter when trying to improve nurses’ knowledge and utilization of capnography. These themes offer an academic, logical, and rational discussion of reviews on nurses’ use of capnography as part of clinical practice in relation to patient management during cardiopulmonary resuscitation. They include subsections that discuss alternatives to capnography, nurses’ attitudes to CPR and capnography, and the impact of change on nurses and patient outcomes.
Background of capnography
People with cardiac and pulmonary issues who are intubated with the use of capnography have been shown to have a more positive outcomes during CPR (Bullock, Dodington, Donoghue, & Langhan, 2017; Chicote, et al. 2019). With the changing healthcare landscape, capnography use in ICUs during the time of intubation has been recognized as beneficial by the (Panchal et al., 2019); moreover, the AHA has recommended it as the standard of care for intubated patients during CPR. Capnography has been recognized in the literature as superior to standard monitoring required such as non-invasive blood pressure, pulse or heart rate monitoring, pulse oximetry, and respiratory rate during CPR (Bullock et al., 2017; Chicote, et al. 2019). The purpose of capnography is to guide the effort of intubation.
Monitoring ETCO2 has been recommended by the AHA (2019) for several reasons. The first is to confirm proper endotracheal tube placement, assess efficiency of chest compression, and gauge the return of spontaneous circulation. ETCO2 is defined as the amount of carbon dioxide (CO2) present at the end of exhalation (Panchal et al., 2019). The normal level is 35-45 millimeter of mercury (mmHg), and the ETCO2 level reflects cardiac output during resuscitation, thereby providing feedback in real-time (Panchal et al., 2019). For example, a decrease in ECTO2 may indicate ineffective compression, ineffective rate and depth of compression, or compression fatigue (Panchal et al., 2019). Capnography measures ETCO2, and as a prognostic tool it provides critical information for assessing a patient’s condition during CPR – capnography allows for gauging the changes in the patient’s condition in real-time (Cook & Harrop-Griffiths, 2019). An ETCO2 level less than 10 mmHg reflects poor cardiac output and strongly predicts unsuccessful resuscitation (Panchal et al., 2019). After 20 minutes of CPR, it is associated with less than 0.5% likelihood of achieving ROSC (Panchal et al., 2019). According to AHA guidelines, a sudden and sustained increased in ETCO2 to normal value during CPR is a strong indicator of achieving ROSC (Panchal et al., 2019). By recognizing ROSC before checking for a pulse, interruptions in chest compression can be minimized.
In the United States, the AHA advised capnography be used during CPR (Panchal et al., 2019). In Europe, the National Audit Project 4 (NAP4) guidelines, which are published for medical institutions both in Europe and the United Kingdom, made the use of capnography or patients subjected to anesthesia regardless of the devices used for airway support (Kerslake & Kelly, 2016; Soar et al., 2015; Link et al., 2015). Additionally, patients receiving advanced life support should also receive continuous capnography monitoring to detect any life-threatening changes (Panchal et al., 2019). While these recommendations suggest that capnography can be helpful in preventing mortality or airway complications in patients within varied clinical settings, the use of capnography during resuscitation procedures has been shown to require additional exploration (Kerslake & Kelly, 2016).
In Kalenda’s (1978) seminal work, the focus was on providing an overview of capnography as an instrument. It was first applied for patients under anesthesia to monitor their coronary condition in the sedated state (Kalenda, 1978). Kalenda (1978) suggested that monitoring pulmonary perfusion during cardiac massage performed for patient resuscitation enhanced the outcomes. The patient cases presented by Kalenda (1978) suggested that changing resuscitating strategies reduces patient mortality rates. This article showed that the presence of a capnography tool allows nurses to control the CPR process more accurately and adjust the cardiac massage as necessary, affecting the efficiency of the resuscitation efforts. While the evidence that supported the use of capnography during CPR was first published in 1978, recent articles show similar findings (Kalenda, 1978).
For example, Hartmann et al. (2015) suggested that applying capnography during resuscitation helps decrease mortality rates. Hartmann et al. (2015) presented a systematic review and meta-analysis of the evidence showing what role ETCO2 measurements play in CPR. Their review considered 27 studies and found that the transparency offered by capnography allowed nurses to see the threshold for ETCO2 objectives during resuscitation. This analysis revealed the important of capnography in supporting the success of CPR and patient outcomes.
The article by Gutiérrez et al. (2018) explored how capnography use during CPR can be enhanced to report more reliable data. In this text, one can see that the positive impact of capnography is undisputed. The authors collected cardiac arrest defibrillator recordings with capnograms and compared the performance of algorithms with and without a filter for capnography. They found a way to make capnography show more accurate data to increase positive patient outcomes, further arguing that capnography is a valuable tool for the procedure of resuscitation (Gutiérrez et al., 2018). It should be noted that other studies, such as the one by Lampe (2017), also advocated for improving the process of monitoring ventilation using capnography.
Capnography is not the only method for evaluating these vital signs, but it is more efficient when compared to others, which impacts the quality of care and is especially crucial during CPR when timing and efficiency of actions can affect the likelihood of survival (Gravenstein et al., 2011). According to Gravenstein et al. (2011), capnography is “the continuous recording of CO2 partial pressure [pp] in inspiratory and expiratory gases” (p. 418). An alternate to capnography – capnometry – does exist; however, it does not provide an opportunity to monitor a patient’s CO2 levels, instead of giving a numerical assessment at a given point in time (Gravenstein et al., 2011). Therefore, Gravenstein et al. (2011) conclude that capnometry is less reliable and specific.
In summary, these six articles presented the history of how capnography evolved over the last four decades. Longstanding and new studies reviewed the use of capnography during resuscitation efforts, consistently finding that the information capnography provides to nurses is invaluable to their knowledge about a patient’s coronary health as well as their chances for success (Gravenstein et al., 2011; Gutiérrez et al., 2018). In synthesis, research from the last five decades showed that capnography should be an integral part of the ICU setting (Gutiérrez et al., 2018; Hartmann et al., 2015; Kalenda, 1978). The literature on the history of capnography supported the place of capnography in the ICU.
Capnography use for emergencies and non-emergencies
Examining the scholarly articles on the topic of capnography for other emergencies and non-emergency situations in the hospital setting can help evaluate the current best practices using evidence-based suggestions and help in understanding the methodology and specifics of the chosen approach. While the discussed literature analyzed the utilization of capnography in various settings, further research can help improve the application of this tool in a clinical setting during CPR (Kiekkas et al., 2016). The following articles demonstrated the broad scope of areas to which capnography has been a valuable addition.
In general, capnography is helpful in the operating theatre during anesthesia; this non-operative practice allows the monitoring of patients. According to Pantazopulus et al. (2015), “low ETCO2 levels may indicate hyperventilation, apnea, esophageal intubation, occlusion of the endotracheal tube, leakage in the ventilation system, poor systemic and pulmonary circulation, hypothermia, massive pulmonary embolism, or ineffective chest compressions” (p. 1053). The systematic literature review conducted by the authors outlined two main themes connected to the application of capnography: implementation and interpretation of results (Pantazopulus et al., 2015). The latter was especially relevant for the issue of resuscitation because a nurse or other medical professional must be capable to quickly assess and interpret the results of monitoring to adjust resuscitation or change the inhalation tubes for patients. The use of capnography in ICU resuscitation can improve the number of successful patient cases (Pantazopulus et al., 2015). However, filtering practices allowing medical personnel to receive reliable results from capnography tools must be implemented since fast oscillations connected to chest compressions can obstruct resuscitation (Pantazopulus et al., 2015).
Stites, Surprise, McNiel, Northrop, and De Ruyter (2017) revealed that capnography could reduce the number of opioid-induced respiratory issues. The clinical setting observed by the authors implemented the utilization of capnography, and the outcomes suggested a statistically significant improvement in percutaneous coronary intervention (PCA) efforts. The retrospective analysis conducted by the authors suggested that short-term cohort research is the best practice for approaching the issue (Stites et al., 2017). In their review, the researchers noted that most researchers explored evidence by examining patient records, implying that retrospective studies are conventional approaches for discussing this topic (Stites et al., 2017).
Langham, Li, and Lichtor (2016) considered capnography outside of anesthesia and suggested that children should be monitored using this tool to detect hypoventilation and apnea, which was also supported by Subramani et al. (2017). In this case, Langham et al.’s (2016) cross-sectional study demonstrated the broad application of capnography and its ability to monitor patients whose health is not directly related to anesthesia. The authors found that routine monitoring can improve patient health, thus showing that capnography has many uses, including in the ICU (Langham et al., 2016).
Cereceda-Sánchez and Molina-Mula (2017) reviewed the prospects of using capnography in the emergency department (ED) setting for detecting metabolic changes in patients. They performed a systemic literature review and examined 17 studies focusing on the specifics of capnography. The findings suggested that this tool is efficient and cost-effective, which further demonstrated the need to develop and implement strategies promoting the use of it in the hospital setting (Cereceda-Sánchez & Molina-Mula, 2017).
In synthesis, the three articles demonstrated capnography allows for the monitoring of the concentration of CO2 in the respiratory gases of the patient. In medicine, this tool is sed during anesthesia or in intensive care units, while some newer studies suggested that using capnography ICU can improve patient outcomes in other cases (Cereceda-Sánchez & Molina-Mula, 2017; Langham et al., 2016; Pantazopulus et al., 2015; Stites et al., 2017). Cereceda-Sánchez and Molina-Mula (2017) suggested using capnography to detect metabolic changes. Langham et al. (2016) advised using capnography in a pediatric setting to monitor hypoventilation and apnea. Pantazopulus et al. (2015) provided a wide variety of settings in which to employ capnography, while Stites et al. (2017) focused on opioid-induced respiratory issues. Overall, capnography allows medical personnel to monitor the inhaled and exhaled gases, which, as supported by research, has innumerous benefits for health care.
Capnography and resuscitation
The general theme in the literature is that capnography has a statistically significant impact on patient outcomes in many areas, including during CPR. Studies have shown why capnography is invaluable during resuscitation (Kalenda, 1978). Some of them also introduced this tool to improve the outcomes of CPR and lower the risks related to it (Langham et al., 2016). A specific practice problem identified in the literature was the impact of nurses’ knowledge on the practice of using capnography in ICU during CPR (Gutiérrez et al, 2018).
While capnography is not the only approach for measuring CO2 levels in a clinical setting, it is the most efficient and accurate (Gravenstein et al., 2011). It improves a nurse’s ability to diagnose respiratory issues and mitigate them, which is especially crucial during CPR (Gravenstein et al., 2011). The main usefulness of capnography is this tool’s ability to evaluate CO2 levels, which is useful in determining the production of CO2, lung perfusion, patients’ respiratory patterns, and alveolar ventilation. A similar tool, the capnometer, measures the CO2 concentrations using a gas sample collected from a patient (Kerslake & Kelly, 2016). However, capnography trace or waveform is the graphic representation of results with time and partial CO2 pressure displayed on x- and y-axes (Gravenstein et al., 2011). Hence, it has been concluded that the continuous monitoring that this instrument provides is vital in the context of the CPR (Cook & Garrop-Griffinth, 2019).
Cook and Garrop-Griffinth (2019) argued that the utilization of capnography in varied clinical settings can serve as a measure for preventing deaths. The authors formed their conclusions on a study of contemporary practices applied in hospitals. Their results suggested that a large percentage of individuals are dying due to misplaced tubes or esophageal intubation, which can be prevented by using capnography (Cook & Garrop-Griffinth, 2019). The common reasons cited by the authors are the failure to use capnography and the lack of education about this tool that would allow medical personnel to use it in case of emergencies.
Lui et al. (2016) considered the value of accumulating data about ETCO2 during patient resuscitation in out-of-hospital cardiac arrest cases. The authors performed a cross-sectional study of adults and found that the information that capnography provides can diagnose cardiac arrest and help nurses to determine a patient’s state. Their findings aligned with those of Elola et al. (2019), Sheak et al. (2015) and Gong, Lu, Zhang, Zhang, and Li (2015). This study showed how one’s knowledge of circulation can help with CPR, and the researchers noted that capnography is essential in such procedures, further strengthening the place of this tool in resuscitation efforts.
Capnography can be used to reduce chest compressions when resuscitating patients. This methodology was developed by Leturiondo et al. (2019) and Merckx, Lambert, Cantineau, and Duvaidestin (1992) and incorporated capnography-based chest monitoring tailored for the purposes of cardiopulmonary resuscitation. The issue with the approach currently used in medical establishments is that chest compressions affect the accuracy of automated ventilation detection, which can endanger the patient (Merckx et al., 1992). Leturiondo et al. (2018) developed an algorithm that considered this issue and allowed for detecting insufficiencies in patient ventilation. Hence, the accuracy of results and reliability of capnography affected the outcomes of resuscitation efforts (Ruiz de Gauna et al., 2018). This methodology suggested that while applying capnography during resuscitation helps improve the patient state, more developments and evidence-based research are required to develop practice improvements (Ruiz de Gauna et al., 2018).
Capnography has been demonstrated to be a preventative measure useful in measuring patients’ CO2 levels, but its use during CPR should be researched further (De Caen & Maconochie, 2018). De Caen and Maconochie (2018) argued that “recent systematic reviews suggest, however, that using specific EtCO2 values to guide patient care during adult cardiac arrest is based upon low-quality evidence” (p. 2). Hence, the lack of high-quality literature and reliable data regarding cut-offs and respiratory patterns measured with capnography can explain why the perception of this technique as useful and its use by nurses during CPR is insufficient. Several studies suggested that capnography can be applied when determining the patient’s state upon CPR (Leturiondo et al., 2018); Ruiz de Gauna et al., 2018).
It is also necessary to understand that nurses in different departments can use capnography, and the decision-making process should incorporate a variety of patient-related factors. Bullock et al. (2017) examined patient cases of resuscitation in a pediatric department to identify whether the guidelines from the AHA in 2010 were applicable to the patient population and if the specifics of utilizing capnography depended on patient characteristics. The research methodology involved a retrospective review of charts assessing data such as trauma, sex, age, capnography results, and patient outcomes. The conclusions suggested that the use of capnography in CPR procedures was inadequate since it was applied in only 13% of cases (Bullock et al., 2017). Moreover, the case reports indicated that individuals who had CPR with capnography were more prone to have a spontaneous circulation in comparison to patients who did not receive it (Bullock et al., 2017). The overall duration of CPR procedures was longer in cases with applied capnography, suggesting that this instrument improves the accuracy of patient prognosis (Bullock et al., 2017). This study contributed to this project’s clinical questions as it highlighted the benefits of capnography and the lack of its proper application in hospitals.
In synthesis, the six studies showed how capnography can prevent avoidable deaths due to unsuccessful resuscitation. According to Cook and Garrop-Griffin (2019), “expired carbon dioxide is routinely detectable during the management of patients with recent cardiac arrest, even in the absence of chest compressions” (p. 439). Their findings, and the findings of other studies, provided support for the use of capnography in the ICU (Elola et al., 2019), Sheak et al., 2015; Gong, et al., 2015). However, De Caen and Maconochie (2018) raised the question of why this topic is still the subject of debate and presented some observations about nurses’ perception of capnography as a valuable instrument during CPR.
Nursing knowledge and patient outcomes
Education of medical personnel on capnography use and the interpretation of results has an impact on the use of this tool. While capnography has been used in a clinical setting for almost 50 years, some researchers suggested the need to dedicate more attention toward educating medical personnel to use this method appropriately for monitoring a patient’s health status and detecting possible heart failure (Langham et al., 2017; Long, Koyfman, & Vivirito, 2017). Education on capnography is a vital as it has been shown to ensure that medical professionals can interpret capnography traces adequately (Kerslake & Kelly, 2016). Additionally, education has been shown to improve nurses’ attitudes and perceptions of capnography use during CPR (Kerslake & Kelly, 2016).
Nurses’ knowledge about capnography and other procedures
Nurses and factors relating to their work have a direct impact on patient outcomes, and improvement of practice approaches or hospital environments have been shown to enhance health-related metrics in patients (Darocha et al., 2017). It has been suggested that a variety of factors, including the availability of capnography tools in hospitals, skills that help nurses to use and interpret waveforms, personnel perceptions of the technique, and the overall attitude of a healthcare organization, affect the practice of using capnography in the ICU (Jaffe, 2017; Darocha et al., 2017). Several studies used a mixed methods design, incorporating a qualitative assessment of nurses’ opinions, hospital managers’ perception of capnography, and quantitative analysis of patient data (Gong et al., 2015; Chhajed et al., 2017; Darocha et al., 2017). These findings led to the development of a questionnaire that accounted for all aspects that obstruct or facilitate the utilization of capnography by nurses (Chhajed et al., 201).
Assessment of death associated with failure to apply innovative tools, such as capnography, can provide insight into the severity of the problem of nurses’ negative perceptions. Pantazopoulos et al. (2015) argued that only 20% of patients who receive resuscitation survive despite the recent advancements in the techniques and technology application used to monitor the process and improve the outcomes. Outside the hospital, the statistics suggested a survival rate of only 10% (Pantazopoulos et al., 2015). Hence, determining the issues that contribute to the high mortality and possible best practices to help reduce the number of adverse incidents can provide guidelines for medical practitioners for capnography use (Pantazopoulos et al., 2015).
The ability to use capnography during CPR has been shown to be affected by the technical expertise that enables using innovate instruments and tools, and it is essential to ensure that nurses possess sufficient knowledge to implement capnography in the critical care unit. Wright (2017) noted that “with overwhelming lack of proper training related to new technology devices such capnography, a sound developmental training program regarding the use of capnography can positively affect patient safety and outcomes” (p. 10). The author showed that training is an essential aspect in developing improvement practice suggestions since the ability to use capnography is crucial for adequate measurements of CO2 levels and adjustment of resuscitation strategies in accordance with this assessment.
Saunders et al. (2017) focused on the correlation between education and training and the quality of work displayed by nurses when they use capnography in a hospital setting. Although they did not use this tool during resuscitation in the study’s case, nurses’ training with the instrument was shown to impact their ability to help patients and lower the need for assisted ventilation (Saunders et al., 2017). Thus, one can see how such an aspect as training has clinical value and can impact patient outcomes, and it was suggested to develop and implement education programs that target this problem during CPR.
According to Aramendi et al. (2017), “capnography permits monitoring ventilation, but the chest compressions provided during CPR corrupt the capnogram and compromised the accuracy of automatic ventilation detectors” (p. 41). The authors explored 83 episodes of cardiac arrest both in the hospital setting and outside the clinical setting to determine the best practices for using capnography in resuscitation. The findings suggested that an approach using only a capnography tool can be a valid strategy in the resuscitation process (Aramendi et al., 2017). The explored evidence suggested that practice improvement guidelines should incorporate strategies for educating and training medical personnel to use capnography in emergencies, for instance, when resuscitating a patient in an ICU unit (Aramendi et al., 2017).
As was previously mentioned, some researchers pointed out that the use of capnography as a part of CPR requires additional attention because the waveform can be distorted by chest compressions, indicating a need for additional training for nurses working in ICUs (Leturiondo et al., 2018). Leturiondo et al. (2018) stated that over 70% of waveforms examined in their study were distorted because of resuscitation efforts. This required the development of an algorithm specially tailored towards CPR that would mitigate the impact of chest compressions on capnography results, minimizing the distortion (Leturiondo et al., 2018). The focus of capnography application during resuscitation efforts was on determining whether the endotracheal tube was placed correctly, ensuring that the performed chest compressions were done correctly and detecting ROSC. Additionally, Leturiondo et al. (2018) argued that capnography could be utilized to develop a prognosis for patients. Ventilation rate monitoring was essential during CPR because it helped nurses detect hyperventilation and prevent adverse patient events.
In one study, Ristagno et al. (2015) inspected data from 1,617 patients with ventricular fibrillation and found that, in general, visual inspection of the waveform was enough for tracking breathing patterns of individuals. According to the researchers, the reliability of results produced through capnography during CRP can be questioned because of distortion. They determined it was necessary to conduct further research. This article presented some potential risks of using capnography without sufficient training, explaining the potential hesitation of nurses toward this change project and laying some groundwork for the first step of the project intervention.
In synthesis, the seven articles explored the relationships between nurses’ knowledge about capnography and its application to the number of adverse outcomes in the ICU, and the information was directly related to the goal of this DPI project. Therefore, the relationship between factors that impact a nurse’s work and professional qualities, such as education or skills, should be explored to determine its significance on capnography use. While alternative approaches to the issue may suggest that the quality of care is facilitated only by the specifics of nurse training, it is evident that other factors contribute as well.
Specific protocols for using capnography
Although capnography as an instrument is not difficult to apply in a clinical setting because it is non-invasive and requires only the presence of a capnography and a medical professional capable of interpreting the results, there a variety of algorithms and strategies for using this instrument. Such a variety of strategies, then, has been shown to complicate nursing training in its use (Panchal et al., 2019). Guidelines for capnography can influence the ways nurses use this tool, and the following articles explore this connection.
Resuscitation-specific capnography utilization
Capnography is a valuable tool that allows for enhancing the process of monitoring a patient’s respiratory function in an emergency scenario, making it relevant during resuscitation attempts (Panchal et al., 2019). Examination of the capnography in the ED were used to inform this project. While the previously discussed literature covered the place of capnography in the process of resuscitation and the guidelines that recommend this tool, scholars have also explored the aspects of this procedure and its application in the ICU.
Haines (2017) examined guidelines and practices used in EDs to provide a qualitative assessment of the capnography application and its benefits. Patients in EDs have been shown to be at a high risk of developing complications because of respiratory function impairment (Haines, 2017). Haines’ (2017) findings were comparable to those of other authors who asserted that capnography is beneficial during CPR since it allows the medical personnel to provide continuous chest compressions without a need to check the patient’s pulse. These findings supported the need for the DPI project as they provided explanations of the application in capnography during CPR and possible reasons demonstrating why this instrument is underused in United States hospitals. Research also showed that capnography is more efficient when compared to other respiratory monitoring techniques (Haines, 2017). For instance, pulse oximetry can be used to detect hypoxia, but the results are not produced continuously (Haines, 2017). Capnography is a non-invasive technique that does not require additional preparations for use, but one should consider different instruments and their appropriateness within the ICU setting (Haines, 2017).
According to Kellshake and Kelly (2016), there are two models for applying capnography tools and measuring the CO2 levels. The first one is a side stream analyzer, which implies taking a sample of gas from the patient’s respiratory tube and placing it in the humidifier filter (Kellshake & Kelly, 2016). This approach has been applied in settings with non-intubated patients because it is more comfortable, and the equipment required for analysis is less bulky (Kellshake & Kelly, 2018). In the second method, mainstream analyzers use infrared light that scans the ventilation circuit. This method has been found to be more suitable for monitoring patients during resuscitation (Kellshake & Kelly, 2018).
Some researchers explored the different combinations of tools and techniques to develop a best practice for applying capnography, which can be used in practice improvement. Salen et al. (2001) explored the possibility of combining capnography tools with a cardiac sonographer in order to improve the procedure of patient resuscitation. The objective was to measure the accuracy of predicting resuscitation outcomes using the two instruments in the ED. The combination did not provide significant improvements, but capnography was shown to be a major predictor of survival for cardiac patients (Salen et al., 2001). Thus, its use in resuscitation is supported further by this research.
In synthesis, there exists an abundance of research that shows how capnography helps during resuscitation. However, many studies have noted the difficulties related to this procedure (Leturiondo et al., 2018; Ristagno et al., 2015). While it is non-invasive, it requires sufficient experience and knowledge from nurses to produce successful outcomes (Salen et al., 2001). These findings lead into the next subtheme: the necessity of education for nurses to improve the use of capnography in the ICU, particularly during resuscitation.
Education to widen capnography use
The focus of this practice improvement project was on intensive care units and resuscitation, but the overview of capnography history revealed how it has been applied in other hospital units, and it is from those units that standard guidelines for using capnography in a clinical setting were established (Panchal et al., 2019). In general, capnography is usually utilized during anesthesia to monitor a patient’s respiratory functioning. Only in recent years have researchers and practitioners begun exploring the implications and benefits of using this monitoring tool in other hospital units. This finding demonstrated the gap in the literature that this DPI project helped to fill: how capnography can be implemented into the ICU.
Kerslake and Kelly (2016) stated that “capnography can be used both for intubated and non-intubated patients” (p. 178). The diversity of metrics that can be assessed using capnography presented an understanding of the need to dedicate special attention to educating medical personnel about how and when to use capnography and how to interpret the results (Kerslake & Kelly, 2016). According to Kerslake and Kelly (2016), capnography “can be used to detect displaced tracheal tubes and tracheostomy tubes and to diagnose inadvertent esophageal intubation” (p. 178). Additionally, the authors argued that this method can be applied to monitor the cardiovascular functions of a human’s body.
Turle et al. (2015) suggested applying automated respiratory monitoring with specific algorithms that help disregard the impact of chest compressions of capnography results. Their methodology, questionnaires, and telephone conversations informed the approach chosen for this DPI. Out of 211 establishments, only four did not have the equipment necessary to conduct capnography assessment, and only 50% of respondents stated that capnography was used to measure the efficiency of CPR (Turle et al., 2015). These findings indicated the inefficiency of use connected to capnography utilization in United Kingdom hospitals. In addition, this study suggested that most establishments lacked the necessary equipment to perform the measurement in general wards (Turle et al., 2015). Arguably, the application of such a strategy would require an even more in-depth knowledge of technology from nurses who would use this instrument in their practice during CPRs.
Nurses’ ability to accurately identify patterns and interpret waveform results can help in preventing adverse respiratory events. Pantazopoulos et al. (2015) stated that “airway management, compression depth and chest recoil, hands-off time, and early defibrillation” are the critical measurements that capnography helps to assess (p. 1053). Airway management was the primary emphasis of this project since it can be used to adjust other elements of resuscitation efforts. However, Pantazopoulos et al. (2015) suggested that current guidelines on monitoring the CO2 levels in a patient gas sample lack clarity and require further examination for the development of best practices. Monitoring end-tidal CO2 has been used as a form of best practice (Panchal et al., 2019). Therefore, the literature supported the need for this project because the evidence suggested that a large number of healthcare professionals lack an understanding of how capnography can improve patient care during resuscitation and affect mortality rates (Haines, 2017; Pantazopoulos et al., 2015).
Zito, Berardinelli, Butler, Morrison, and Albert (2019) focused their attention on how nurses use capnography results to make decisions regarding patient discharges, using confidence levels assessment. This cross-sectional study observed 133 patients before and after ETCO2 assessments and measured nurses’ perception of the patients’ readiness for discharge. In the study, it was evident that nurses changed their prognoses based on the outcomes of ETCO2 levels assessment. As was previously mentioned, even though capnography is mainly applied in the operating theater, most cases of airway complications occur outside this setting. Hence, there existed a need to evaluate the number of such cases and the readiness of nurses to apply capnography in the ICU unit.
An essential aspect of this project was the need to accurately assess and measure nurses’ knowledge of capnography use in the ICU setting to be able to compare the two variables. Kiekkas et al. (2016) developed a questionnaire titled Nurses’ Knowledge about Capnography Test (NKCT). The questions incorporated in this assessment aim to evaluate nurses’ understanding of capnography functions, aspects of ETCO2 levels, waveform interpretation, and specifics of using capnography in a clinical setting (Kiekkas et al., 2016). The NKCT is a relatively new tool; thus, only one study that employed this test to measure nurses’ knowledge of capnography has been identified (Wright, 2017).
In synthesis, these six articles focused explicitly on emergencies and the prospects of using capnography to improve patient outcomes. The literature suggested that capnography can significantly improve the current practices of resuscitation and CPR (Haines, 2017; Kerslake & Kelly, 2016; Panchal et al., 2019). According to the European Resuscitation Council, capnography use enables the detection of ROSC “without pausing continuous chest compressions thereby improving quality of resuscitation and preventing the potential harm caused by administering a further bolus of adrenaline after ROSC” (as cited in Kerslake & Kelly, 2016, p. 180). Therefore, nurses must possess the knowledge regarding capnography to use it appropriately during resuscitation activities and must have the ability to recognize vital signs associated with ROSC.
Barriers to using capnography
As noted above, the complexity of using capnography outside of its usual setting is based not only on the tool itself or its availability in the hospital, but also nurses’ hesitancy in following new evidence and recommendations. While American and international guidelines have recommended that capnography as a valuable addition to the process of resuscitation, the number of cases where it is used remains low (Aramendi et al., 2017). Therefore, one has to look at possible barriers to capnography use outside of resource unavailability.
According to Aramendi et al. (2018), capnography use is challenging as not all nurses can see the exact differences between breaths and chest compressions. The researchers were able to develop algorithms that allowed medical personnel to use programs in a more advanced way for determining the location of ventilation during resuscitation activities. This study had several implications for the project. The findings implied the need to improve nurses’ current knowledge about capnography by providing them with the described algorithm. The algorithm would help enhance nurses’ confidence in using the technique, thereby improving patient outcomes (Aramendi et al., 2018). Additionally, this would improve the CRP process in general by mitigating risks of hyperventilation, which is often associated with adverse patient outcomes (Aramendi et al., 2018).
Nassar and Kerber (2017) argued that despite the significant prevalence of poor outcomes associated with CPR and a large volume of evidence-based research providing guidelines regarding best practices within this domain, the adherence to these suggestions in clinical settings remains low. Nassar and Kerber (2017) stated that “feedback devices provide instantaneous guidance to the rescuer, improve rescuer technique, and could impact patient outcomes” (p. 1061). The authors used a systematic review and listed several elements that contributed to the improvement of CPR practices in previous projects. They stated that capnography is a critical aspect in monitoring chest compression and tracking the return of spontaneous circulation. This suggestion supported the primary claim of this DPI and highlighted the need to determine what factors impact the lack of capnography application during CPR and the development of interventions that can address these problems.
The previous study suggested that the prevalence of capnography use among nurses use during CPR remains low. However, it is possible that other factors, apart from knowledge and perception, obstruct the adoption of this respiration-monitoring tool. Sahyoun, Siliciano, and Kessler (2018) developed a questionnaire for hospital managers to examine whether the hospitals in New York City had equipment that would allow them to use capnography during resuscitation. Sahyoun et al. (2018) stated that 95% of the respondents had the devices that allowed their personnel to monitor ETCO2, and 97% of those implemented a protocol for applying them. However, only 54% reported having a protocol tailored explicitly for CPR, which is consistent with the findings of studies by Dioso (2017). Thus, despite the availability of capnography, hospital personnel may have difficulty applying these tools because no protocols or guidelines are established at the sites to help them determine how to use it.
One can argue that the lack of guidelines and efforts dedicated to ensuring that hospitals use capnography may harm patients due to inconsistency of practice and care. Carlisle (2015) aimed to develop a standardized protocol for using capnography during resuscitation for opioid-induced respiratory depression (OIRD). This article explicitly targeted nurses and their ability to use the tool during CPR. The author noted the absence of education as a problem leading to nurses’ resistance to using the guidelines.
Hassankhani et al. (2015) cited education as a vital factor for promoting the utilization of capnography in a clinical setting. The findings were based on the nurse interviews regarding the application of the protocol. The answers suggested that the issues are connected not only to the availability of devices and to the system issues but also to the lack of nurses’ education and patient adherence. Therefore, Hassankhani et al. (2015) concluded that learning played a vital in the success of implementing capnography in a clinical setting.
Whitaker and Benson (2016) indicated that approximately 74% of deaths in ICU could be prevented if capnography monitoring was implemented as standard practice. The primary goal of this strategy is to improve patient safety. Hence, Whitaker and Benson (2016) also recommended using a standardized protocol and providing nurses with additional training. Such education would fill the gaps in knowledge and understanding of the interpretation of capnography.
Kodali and Urman (2014) suggested that the universal application of this tool during CPR would allow for the creation of a database of waveforms that could be utilized to improve the existing capnography protocols. Hence, the promotion of using this methodology would help to further enhance the practice of capnography during CPR. Kodali and Urman (2014) conducted a literature search to locate evidence supporting the benefits of capnography in resuscitation published from 1960 until the present and concluded that, historically, the interpretation of outcomes and attitudes regarding the predictions and evaluations that can be made using this approach changed since it was accepted that the “presence of small obtunded CO2 waveforms during CPR reinforces tracheal location of an endotracheal tube” (p. 332). In general, capnography use during resuscitation requires the knowledge of not only waveform interpretation but also the understanding of distortions caused by CPR. The complexity of using capnography during resuscitation can be a crucial factor contributing to nurses’ lack of confidence when using capnography, especially in emergency cases (Kodali & Urman, 2014).
In synthesis, the seven in academic research theme demonstrated several barriers that nurses encounter when using capnography during CPR. The most important one was the lack of nurses’ training in capnography, which resulted in other problems that arise when a hospital or unit wants to implement practice changes (Dioso, 2017; Sahyoun et al., 2018). Moreover, the lack of standardized data has been shown to further increase nurses’ resistance to change in regard to capnography use (Kodali & Urman, 2014), which revealed a gap in practice that the project attempted to fill.
Summary
Overall, the problem that this project explored was the practice of using capnography in the ICU setting during patient resuscitation and the impact of nurses’ knowledge about the tool on the prevalence of use and CPR outcomes. The origin of the issue was connected to evidence presented by scholars, suggesting that nurses both in the United States and Europe do not apply capnography to guide cardiac massage and track respiratory patterns of patients despite the wide availability of capnography tools (Wright, 2017). This project aimed to improve the lack of understanding associated with the perception and knowledge of capnography utilization and patient outcomes. This project was similar to the study by Sahyoun, Siliciano, and Kessler (2018) who aimed to examine the problem of knowledge about capnography, perception, and the frequency of application. However, their sample size was little, suggesting that more attention should be dedicated to the problem of correlation between knowledge and application in capnography use. The current literature lacked quantitative studies on nurses’ knowledge and capnography use (Kiekkas et al., 2016), demonstrating the need for this DPI project.
The empirical evidence on the topic of capnography suggested that in most cases, using capnography during CPR improves the accuracy of cardiac massage and survival chances (Haines, 2017; Kerslake & Kelly, 2016; Panchal et al., 2019). The problem has evolved since initially capnography was developed as an instrument applied during anesthesia, but current trends have suggested that capnography and standardized protocols for its use it can improve care in many healthcare domains (Jooste et al., 2019). However, the ability to use capnography has been shown to be obstructed by nurses’ lack of knowledge and training (Kodali & Urman, 2014). Since capnography allows medical professionals to monitor a patient’s well-being in the ICUs, nurses in these units should receive not only protocols or guidelines but also adequate training on capnography (Kodali & Urman, 2014).
In general, the application of capnography across different domains of patient care becomes more popular. The main trends in applying capnography for patient monitoring within the ICU settings are connected to the promotion of using this tool and improvement of the interpretation of results which can be obstructed by distortions (Aramendi et al., 2017; Chicote et al., 2019). The primary trend that prevails in the literature was the adoption of capnography for use in different medical settings, including the ICU. The expansion of the use for this instrument suggested that many hospitals may begin to have capnography available at each ward, further emphasizing the need to examine personnel’s ability to use this tool correctly (Kerslake & Kelly, 2016). In addition, many researchers have developed specific algorithms, including computer programs, that help enhance the interpretation of results or automate the process of monitoring using capnography (Chicote et al., 2019). The general trend, as shown in the literature, is toward the application of capnography across different units and the improvement of application strategies (Kodali & Urman, 2014; Panchal et al., 2019).
Many previous studies were based on small research samples of 20 to 30 nurses or patients, which can mean under-representation (Dioso, 2014; Jooste et al., 2019). The authors generalized the findings to create a conclusion based on the evidence they collect (Kerslake & Kelly, 2019; Jooste et al., 2019). From this perspective, evidence supporting the efficiency of using capnography in the ICU during resuscitation might not be justified. However, other studies have focused on exploring patient records to determine the effect of resuscitation using capnography on mortality, and so incorporated enough data samples (Aramendi et al., 2017; Kodali & Urman, 2014). Yet, these conflicts in methodology have led to few quantitative studies that assess the availability of capnography tools, the number of cases where it was applied, and outcomes.
Hence, a significant gap in the literature is the lack of evidence that would provide an understanding of nurses’ knowledge of capnography and attitudes towards using this tool. Prior research was done on the topic that explored the prevalence and specifics of nurses using capnography and suggested that, in most cases, this instrument is not applied during CPR despite recommendations (Dioso, 2014). This gap in practice led to the development and informed this DPI project, which explored nurses’ knowledge, capnography use during CPR, and patient mortality, and the connection between these variables in a quantitative fashion. Most of the examined studies focus on the advances of using capnography and the specifics of its application (Kerslake & Kelly, 2016). Additionally, the literature demonstrated that there existed a gap in nurses’ knowledge on capnography use, leading to negative perceptions on the tool’s usefulness, which further demonstrated the need for the DPI project which assessed how changes in nurses’ knowledge about capnography affected ROSC (Aramendi et al., 2017).
Two theoretical frameworks informed the implementation of the project at the practice site. The first was Tanner’s (2006) clinical judgment model. This model introduced the four phases of how nurses make clinical judgments – noticing, interpreting, responding, and judging (Tanner, 2006). These steps imply that, after noticing a problem, collect and analyze data based on their knowledge and logic and make clinical decisions to act, monitor patients, or collect more data. In the end, nurses reflect on their choices in order to improve the process of clinical judgment and deliver better results in the future (Tanner, 2006). Tanner’s model gave the project a foundation for how nurses made choices based on their knowledge of tools and procedures.
The second was Lewin’s change model. Lewin’s model was used due to the gaps identified in the literature review. It was apparent in the literature that the equipment for capnography is present in most hospitals and enough data exists to support the use of this tool during resuscitation (Lewin, 1951). However, the rates of using this instrument have remained low, and nurses have expressed hesitations on its use (Lewin, 1951). Thus, a change theory in which people’s fear of and resistance to change was necessary. Lewin’s model offered a simple theoretical base that showed how these obstacles could be overcome.
The quantitative, quasi-experimental methodology was chosen to connect patient outcomes and nurses’ use of capnography in a calculable, transparent way. The main goal was to determine the degree to which capnography use during resuscitation impacted patient outcomes and nurses’ subsequent implementation of this tool in the unit. The strategy chosen for this DPI is based on the previous studies. The research related to the use of capnography in a clinical setting employed questionnaires and knowledge tests. Moreover, data, such as mortality rates, is often used; thus, these two approaches are united in the present DPI to deliver appropriate results.
Chapter 3 will focus on exploring the clinical question and on the methodology used for this DPI that was based on findings from the literature. Chapter 4 will present the results of data collection and analysis. Finally, Chapter 5 will present the interpretation of the project findings as well as discussion the implications of the results. Additionally, recommendations for future projects and practice will be made.
Methodology
This DPI project focused on the use of capnography during CPR by nurses, linking their knowledge of capnography techniques and the application of capnography within an intensive care unit (ICU). A quantitative method was chosen to explore the relationship between nursing knowledge of the utilization of capnography and how its usage during CPR would lead to positive patient outcomes within intensive care units (ICUs). The clinical questions guiding this project were:
- Q1: Does the implementation of the AHA Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care impact nurses’ knowledge of capnography, compared to current practice, among ICU nurses in an acute care hospital in Southern New Jersey over four weeks?
- Q2: Does the implementation of the American Heart Association’s Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care for Emergency Care impact the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest in an acute care hospital in Southern New Jersey over four weeks?
The purpose of this quantitative, quasi-experimental project was to determine if and to what degree the implementation of the AHA Guidelines for Cardiopulmonary Resuscitation would impact nurses’ knowledge of capnography and the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest when compared to current practice at a 20-bed ICU in an acute care hospital in Southern New Jersey over four weeks. Improving nursing knowledge in capnography was essential for increasing the quality of care and resuscitation efforts at the project site. Nurses’ knowledge may also aid in generating positive outcomes for patient success rates and promoting increased patient outcomes.
Chapter 3 provides a discussion on the methodology that was used to implement this DPI project. The population and sample selection are discussed as are the selected instruments and data collection approaches. The validity and reliability of data collection tools are validated, which supported the project’s data collection procedures and data analysis processes. The chapter ends with discussions on bias mitigation, ethical concerns, and project limitations.
Statement of the Problem
The AHA’s Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care recommended the use of capnography for measuring ETCO2 to assess and measure return of spontaneous circulation (ROSC) (Panchal et al., 2019). It was not known if or to what degree the implementation of the American Heart Association’s (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Emergency Care would impact nurses’ knowledge of capnography and increase the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest when compared to current practice in urban New Jersey. Nurses working in intensive care units, where the risk of cardiac arrest is high, are required to use evidence-based tools and strategies to reduce patient mortality (Israel, 2014; Jaffe, 2017). Capnography has been shown to provide details about a patient’s condition and assist care providers in tracking changes in a patient’s condition to avoid complications (Heradstveit & Heltne, 2014; Pantazopoulos et al., 2015). Capnography has proved to be effective in promoting increased patient outcomes in the detection of abnormalities associated with fluctuations in CO2 levels and following cardiac arrests (Cereceda-Sánchez & Molina-Mula, 2017; Chhajed et al., 2016; Darocha et al., 2017; Hassankhani, et al., 2015).
The widespread application of capnography during resuscitation attempts within specific clinical settings has yet to be achieved due to the lack of specialized training that focuses on the tool and understanding of its use (Dioso, 2014; Duckworth, 2017). This subject has not been addressed in the literature since most studies focused on the various applications and benefits of capnography (Chhajed et al., 2016; Darocha et al., 2017). Hence, it was not known whether increased nurses’ knowledge of capnography is associated with improved use of this tool during cardiopulmonary resuscitation.
The problem affected various patient populations who are at-risk of a cardiac arrest, including patients in intensive care units as well as those with chronic cardiovascular conditions. The barriers to consistent implementation of capnography use within a critical care setting prevent care providers from delivering the highest quality of care, thus posing a risk for patients’ survival during a cardiac arrest. Hence, it was essential to explore the factors that could hinder the use of capnography in high-risk settings as this would help to develop evidence-based strategies to enhance capnography use. Evidence of a positive relationship between nurses’ knowledge of capnography, their readiness to use this tool, and the rate ROSC as a result of resuscitation following cardiac arrest would help to fill the gap in current literature, thereby expanding on the significance of these techniques.
Clinical Questions
The clinical questions answered in this project were:
- Q1: Does the implementation of the AHA Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care impact nurses’ knowledge of capnography, compared to current practice, among ICU nurses in an acute care hospital in Southern New Jersey over four weeks?
- Q2: Does the implementation of the American Heart Association’s Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care for Emergency Care impact the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest in an acute care hospital in Southern New Jersey over four weeks?
These clinical questions represented the independent and dependent variables that were explored in this DPI project. Two groups of patients from two different time frames were compared before (comparative group) and after (post-implementation group) of the project. The independent variable was the educational intervention based on the American Heart Association’s (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care (Panchal et al., 2019), specifically the use of capnography during CPR, and the dependent variables were nurses’ knowledge of capnography measured by the Nurses’ Knowledge of Capnography Test (Kiekkas et al., 2016) and ROSC, which was obtained from the facility Code Blue data, specifically in the documentation of end-tidal CO2 during CPR. Data were extracted from the Code Blue records by the quality improved nurse and delivered to the investigator and de-identified. Then, this information was entered to an Excel spreadsheet by the primary investigator.
The project’s methodology was quantitative, and both dependent variables were represented by numbers. An existing instrument was used to measure nurses’ knowledge of capnography. Designed by Kiekkas et al. (2016), the Nurses’ Knowledge about Capnography Test (NKCT) provided a validated test for collecting data about the outcomes of the proposed intervention and the knowledge that nurses in the ICU possessed about using capnography (see Appendix B). The quasi-experimental design was selected as it aligned with the first clinical question, and its questions directly addressed nurses’ potential hesitation and overall preparedness for using capnography during CPR. For the other dependent variable on ROSC rates, data were pulled from the Electronic Health Records (EHRs) as it contained all necessary information about patients residing at the unit, the number of codes the unit had in regards to CPR, and how many times the use of capnography during resuscitation was registered.
Project Methodology
The methodology selected for the project was quantitative; this was justified by the need to explore the subject from an objective viewpoint. The primary benefits of quantitative methods are that they provide accurate numerical information, reducing the risk of bias (Gunnell, 2016). The quantitative methodology incorporates mathematical, statistical, and numerical analysis of gathered data using computational techniques (Valente & MacKinnon, 2017). In quantitative methodologies, the information can be collected with the help of surveys, questionnaires, and by using existing statistical data or health records and manipulating it with technology. This methodology provided an opportunity to answer the clinical questions using objective calculations, which could led to data generalization across groups of people.
Additionally, according to Jones (2016), quantitative methods focus on providing a vast scope of information rather than on exploring some variables in-depth. This means that such methods could be useful in settings where there is a need to collect as much information as possible and draw sound conclusions. In the present case, gathering more information was beneficial as it provided more evidence of the impact of the independent variable on the two dependent variables. The data collected in quantitative projects are also simplistic in nature, making this methodology particularly useful for observing changes in variables, analyzing data for correlations, and presenting it for review and replication (Ali & Bhaskar, 2016; Heale & Twycross, 2015; Leppink, O’Sullivan, & Winston, 2016; Watson, 2015).
Quantitative data sources are particularly helpful in obtaining evidence about the effects of one variable on another, which was the primary goal of this project. It is more useful and practical than the alternative, qualitative methodology, for several reasons. In contrast with quantitative data sources, qualitative methods focus on obtaining meaningful information about the participants’ attitudes and beliefs by enhancing the depth of data collected (Austin & Sutton, 2014; Barnham, 2015; Flanagan, Greenfield, Coad, & Neilson, 2015; Gunnell, 2016). Qualitative projects focus on the participants’ perceptions rather than on objective information; they take information that is challenging to measure and draw specific themes based on individual views of the problem and related theories (Gunnell, 2016).
In this DPI project, qualitative methods allowed for the examination of nurses’ beliefs about their own knowledge about the implementation of capnography use during CPR and its importance. This information, however, would not show how an intervention could affect the use of capnography during CPR and patient outcomes connected to the change (Barnham, 2015). The dependent variable of nurses’ knowledge was quantifiable, and the quantitative methodology allowed the investigator to see the relationship between nurses’ training and their decision-making by analyzing the records and nurses’ knowledge. A 30-item survey, Nurses’ Knowledge about Capnography Test NKCT (Kiekkas et al. 2016) was administered at two timepoints: pre and post evidence-based educational intervention (see Appendix B). There was a two-week separating between pre- and post-implementation NKCT surveys. A demographic survey was administered during the two-weeks post-intervention time point.
Similarly, the data on ROSC rates were also numeric and take from the EHRs. Baseline data on ROSC rates were extracted for four weeks before the project and four weeks after implementation of the American Heart Association’s (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Data for the comparative and post-implementation patient groups were collected through chart review of the EHRs. This allowed for the pre-intervention and post-intervention days to be assessed and to answer the clinical question when there was a non-equivalent group (Curtis et al., 2016).
The selected methodology was best suited to answer the clinical questions in two ways. First, it allowed for the objectively evaluation of the level of knowledge about capnography, in contrast with qualitative methods, and established of the impact nursing knowledge had on the practice. Given the nature of the problem at hand, evaluating factual knowledge was more important because it provided more information about the effectiveness of nursing education in capnography. Secondly, quantitative data obtained through the EHRs were more structured, making it easier to analyze how nurses’ knowledge translated into their practice.
Project Design
The chosen design for the quantitative project was quasi-experimental. As explained above, this was the most suitable design for the DPI project and the best fit for answering the clinical questions. A quasi-experimental design is similar to an experimental design in that they both measure the causal impact of an intervention (Alessandri, Zuffianò, & Perinelli, 2017). However, in contrast to pure experiments, this design does not use a randomized population sample, assuming partial or full control over the sample’s selection instead (Alessandri et al., 2017). Moreover, the unique feature of one-group quasi-experimental projects is that they do not use a control group for comparison, using results from one sample group (Alessandri et al., 2017). Thus, the design allows for more control over the project, but some limitations and potential challenges do arise from its use.
A quasi-experimental design was deemed the best fit for the current intervention relies due to its ability to directly address the clinical questions. The clinical questions latter explored the connection between nurses’ knowledge of capnography under the influence of the intervention before and after the program had been implemented and the effect of this initiative on the use of capnography. According to Valente and MacKinnon (2017), the aim of quasi-experimental projects is to examine the impact of such change programs. Furthermore, the increased attention to choosing the sample implied the ability of the investigator to use their desired setting for the project and see how the intervention affected specific populations. In this case, the nurses’ participation in training made them a necessary part of the project. At the same time, only patients who experienced cardiac arrest and required CPR were eligible for the project, and randomization of the sample seems inconvenient for exploring the clinical questions.
The role of quasi-experimental design is apparent in the variables outlined in the project as the number of resuscitations with the use of capnography before and after the intervention requires a highly specific set of patients in the hospital, the examination of which would be impossible when using other quantitative designs. Similarly, the chosen design explains the use of quantitative methodology and shows how numerical values can be utilized to answer the clinical question. Thus, this design further supported the use of quantitative methodology as opposed to qualitative or mixed varieties.
Two sets of data were collected for examination based on the quasi-experimental design. The first was the nurse’s knowledge of capnography, which was collected using the NKCT. The NKCT was used in a pre- and post-test fashion to demonstrate the effect of an educational intervention, a training program for nurses about capnography use in resuscitation, on the nurse participants knowledge. The second dataset was pulled from the EHR data about codes that showed the cases of resuscitation in the unit and the use of capnography during these codes for four weeks before and four weeks after the intervention was implemented. The quasi-experimental design allowed the investigator to collect data at points before and after the intervention to compare them to demonstrate the effect of change and its significance.
Population and Sample Selection
The setting for the intervention was the 20-bed ICU of a hospital located in Southern New Jersey where nurses are under increased pressure to deliver timely care and respond to situations that pose a significant risk to patients’ health. The ICU was chosen because these units have many patients whose health can deteriorate or change rapidly, and they require constant attention and monitoring. Nurses working in the ICU must act quickly, assisting patients in an environment where each decision may be crucial to their health. Moreover, there is a high incidence of cardiac arrests in the ICU, and thus, nurses are often involved in cardiopulmonary resuscitation (Wright, 2017). The combination of these factors emphasized the need for the proposed intervention since it would increase the quality of care. As a result, the project’s results also presented an opportunity for improvement and potential benefits for other units and locations.
The department under examination was a 20-bed unit in which 32 nurses are employed. While the unit is licensed for 20 beds, it operated at an eight- to ten-bed capacity during the project time frame. While nurses working at the ICU were not the population for the project, this number shows the amount of preparation for training. For instance, this number demonstrated the capacity of nurses to perform CPR and respond to patients’ needs as well as how many days were required to implement the training program and assess nurses’ knowledge of capnography.
The project population included all patients who were treated at the selected ICU during the project implementation. The sample for the project was patients who experienced cardiac arrest and underwent resuscitation in the intensive care unit of the selected location. The inclusion criteria for the sample were patients who were treated in the selected unit at the time of the project. Moreover, these patients must have experienced the code situation (cardiac arrest) and underwent CPR as a result. Exclusion criteria for the sample were patients under 18 years old. Only adult patients who were older than 18 at the time of the project implementation were considered to deliver results that could be generalized for a larger adult population (Mohamed, 2019). Furthermore, patients who had a cardiac arrest but did not undergo resuscitation were also excluded. Reasons for not performing CPR could include a Do Not Resuscitate (DNR) order.
The size of the sample for patient CPR cases could not be determined pre-emptively as the number of cardiac arrests was not a measure that could be predicted. The conclusive records about the code situation and the use of capnography could only be obtained only after the period of the intervention was over, thus finalizing the project sample size only after the four-week duration of the project. Nevertheless, the sample size was not controlled or restricted, thus demonstrating the flow of patients and case situations in an environment without the investigator’s influence. The number of nurses who needed to complete the NKCT was 32 as all nurses in the unit were required to attend the educational training on capnography.
The selected sample size was rather small for a quantitative project because this design implies collecting data from as many charts and participants as possible (Cronin et al., 2014). This meant the size of the sample in this project was constricted by the geographical location of the project and the focus on intensive care units, which limited the number of cases available for the project. The selected sample size was enough for a quasi-experimental design (Cronin et al., 2014). Moreover, the focus on ICUs allowed for a discussion on the connection between the specific department’s setting and nurses’ skill and their treatment of patients. An a priori power analysis was conducted using G*Power 3.1.9.7 software and yielded a suggested sample size of 15 nurses based on a two-tailed paired t-test with 80% power, alpha set to.05, and a large effect size (.80).
The geographic specifications of the project meant that nurses were recruited from a single state; in this case, Southern New Jersey, where the evaluation of this DPI improvement project was performed. Nurses did not have to travel to take the test; instead, all data collection procedures were conducted at their place of work in a way that did not impair the workflow. Similarly, patients were not disturbed to gather data about cases of cardiac arrest as the EHR was the main source of information. All data were anonymized to remove identifying information such as names and occupations.
Instrumentation and Sources of Data
There were two dependent variables for which data was collected –nurses’ knowledge of capnography and the number of CPR cases with the use of capnography. The type of data for all variables were quantitative but came from two different sources. This separation of the instrument and a source of data was required to show the effect of the intervention on the use of capnography.
The Nurses’ Knowledge about Capnography Test (NKCT). The NKCT was used to collect the required data on the nurses’ knowledge of capnography. This tool was developed by Kiekkas et al. (2016) and included 30 correct and wrong statements about capnography (see Appendix B). The items are separated into four groups: principles of capnography function, conditions affecting ETCO2 pressure, conditions affecting capnography waveform, and indications for capnography use (Kiekkas et al., 2016). The test was delivered to all nurses identified through probability sampling (all nurses working at the selected ICU) and marked on correctness to determine the level of capnography knowledge. The test contains 30 items, which are formulated as correct and incorrect statements about capnography use. The nurse taking the test chooses whether each statement is true or false, and the results of the tool are quantitative. The NKCT is an established tool for appraising nurses’ knowledge of capnography, thus making it an appropriate selection for this project as a test with proven results (Kiekkas et al., 2016).
The Electronic Health Record (EHR). The second source of data was the EHRs of the selected ICU, which contains information about the patients treated at the hospital in that unit. The records document patients’ descriptions, including their age, gender, and ethnicity, which were collected to make the dataset more informative. The primary type of data, however, was the number of cardiac arrests and resuscitations with and without the use of capnography. The data were collected and stored electronically in an Excel spreadsheet to ensure that each instance was properly documented. The number of code situations with CPR were recorded as a cardinal number, and each instance of CPR had a descriptor of “1” and “0” to denote the use or non-use of capnography. Thus, the final type of data was a ratio.
Electronic health records have high validity and reliability as health records are the main place for the hospital to gather all data related to patients’ health (Lin et al., 2018). It is an official source of information that is handled by the staff, which implies that all code situations must be in one place. The permission from the hospital to collect and use data was obtained, and the data was anonymized to ensure participant’s privacy – patient’s names were replaced with numbers, and only their age, gender, and ethnicity were collected to avoid potential identification.
Validity
Validity is the quality of a measurement or concept regarding their correspondence with the real world. In research studies, validity is checked for measurement tools in order to test their accuracy of measuring data (Heale & Twycross, 2015). The description of validity explains why it is important in academic projects – validity for measurements ensures that the instrument used during data analysis will yield results that adequately represent the events that happen in real life.
The NKCT has been evaluated for construct validity using techniques designed to test the relationship between the NKCT and the knowledge base of nurses in capnography (Kiekkas et al., 2016). The authors used nurses’ experiences in the anesthesiology department and the date of introduction of capnography to the said department to determine nurses’ capnography experience, and education levels were derived from nurses’ qualifications (Kiekkas et al., 2016). The authors concluded that the evaluated construct validity was high because both characteristics had a positive effect on the NKCT scores as predicted (p = 0.038 and p = 0.003, respectively). The use of an instrument with high construct validity ensured that the data collected on nurses’ knowledge also had high validity.
The validity of EHR data depends on the fullness of patient information. According to Lin et al. (2018), high data completeness increases the quality of gathered information and improves the results of the analysis. Most problems arise when projects require patient information from different providers or out-of-hospital situations (Lin et al., 2018). Since the present project used a small part of patient data that pertained to their treatment at the single unit, the validity of the data gathered from the her was high.
The DPI project required only a small set of descriptive characteristics (age, gender, ethnicity) and the code for cardiac arrest and CPR with or without capnography. All needed information was recorded by staff of the department or administrative personnel, and the participation of clinicians outside of the hospital was not necessary to collect these data. Thus, the factor of EHR-continuity did not have a significant influence on the results of the data collection process. The use of the HER validity score developed by Lin et al. (2018) was, therefore, not needed to ensure the fulness of information, as it did not affect the outcomes of data analysis for answering the clinical question.
Reliability
While validity is responsible for measuring tools’ ability to represent real-life data, reliability is the consistency of a measuring instrument (Heale & Twycross, 2015). By checking a tool’s reliability, scholars establish whether this measure produces the same or similar results under established conditions. The importance of high reliability is related to the investigators’ need to replicate studies using the same tools (Heale & Twycross, 2015). A tool that has high reliability increases scholars’ chances of repeating the testing process and obtaining results that are precise, consistent, and representative.
Both the NKCT and the EHR are reliable sources of data, demonstrating that they can be used to provide reliable outcomes. The NKCT’s reliability was evaluated by its creators. Kiekkas et al. (2016) noted that they applied internal consistency and item analysis to determine the reliability of the instrument. A Kuder-Richardson 20 coefficient was used based on the type of the test (dichotomous choices) (Kiekkas et al., 2016). The point-biserial correlation index was also applied, yielding the results from 0.168 (poor item discrimination) to 0.833 (excellent item discrimination) with most items (28 out of 30) having either a good or acceptable discriminatory value (Kiekkas et al., 2016). This means that the internal consistency of the test is high. Therefore, data collected using the NKCT has a high degree of reliability. The internal consistency was supported by intra-rater reliability evaluation. Both tests used by the authors provided an adequate degree of certainty, thereby ensuring the reliability of data collected using this instrument (Kiekkas et al., 2016). Data collected from the EHR were assumed to be reliable as accurate information from Code Blue sheets was documented into the EHR and checked against the Code Blue sheets to maintain reliability.
Data Collection Procedures
Obtaining institutional approval from the selected hospital to conduct tests and observations in intensive care units was the first step prior to data collection and initiated the process. Institutional Review Board (IRB) approval from Grand Canyon University (GCU) was then sought and obtained (see Appendix A). Once the approval from the site and the IRB had been received, a list of all nurses working in the ICU of the selected hospital was obtained. This formed the basis of the project to access the knowledge of nurses’ working in this setting from a quantitative perspective. The nurses involved in the project were contacted by e-mail, and information about the results and findings were explored in detail. The project employed qualitative evaluation of the collected data, using the NKCT and calculations, such as t-tests and Fisher’s exact test. The procedures for data followed the rules that protected participants’ private information and guaranteed confidentiality (Cronin et al., 2014; Price et al., 2017).
The 32 nurses in the 20-bed ICU were then required to attend a training on capnography and the AHA guidelines. Prior to the educational intervention, the nurses took the NKCT pre-test, which demonstrated their pre-education knowledge. Then, two weeks after the educational intervention, the same 32 nurses took the NKCT post-test to determine whether the intervention influenced nurses’ perception of capnography. The NKCT was used to examine how the independent variable, the educational intervention and implementation of the AHA guidelines, impacted the first dependent variable, nurses’ knowledge on capnography. During both the pre- and post-test NKCT surveys, all participating nurses took the test in a controlled environment, a conference room. The test was completed either after the nurses’ shift or before so that it did not disrupt their workflow. For any nurses who had difficulties in scheduling, the test was conducted individually.
Near the completion of the project, after both NKCT surveys were collected, nurses were also asked to complete a short 3-item post-intervention survey. This survey contained 3 statements on the nurses’ perception of knowledge and understanding of capnography use following the educational intervention. The short survey’s items were measured on a Likert scale to collect nurses’ feedback about the project in a quantitative form.
The second part of data collection involved using the hospital’s EHR to gather information about patients and instances of CPR for four weeks pre- and four weeks post-implementation of the project. As noted, a small set of patient descriptors was necessary to make the dataset more informative. Adding such information as patients’ gender, age, and ethnicity presented valuable findings for future studies and showed whether the sample was heterogeneous and suitable for generalization. Moreover, each instance of cardiac arrest with CPR was recorded, and cases that involved capnography were noted in the EHRs on the Code Blue sheet. The pre-implementation data were collected 28 days prior to the start of the program to form a set of comparative baseline data. Post-implementation data were collected at the end of the program, or more specifically, 28 days after the start of the program. As the data were collected from digital records, minimal manipulation was necessary to standardize the information and present it in an Excel spreadsheet.
Neither datasets required informed consent since the intervention involved all nurses, and patient data were collected and de-identified through the EHR. Nonetheless, the agreement with the hospital about the amount and types of data provided ensured that the investigator had access to the necessary information. As mentioned previously, all data were anonymized, and the results of the NKCT and EHR data were coded to exclude any uniquely identifiable information such as names or positions. The data were stored digitally on a password-locked computer at the project site. All data will be destroyed in one year after the end of the project per hospital policy.
Data Analysis Procedures
For the purposes of the present project, data on two variables were collected: nurses’ knowledge of capnography before and after the intervention and the use of capnography during CPR. For the first variable, quantitative data were collected using the Nurses’ Knowledge on Capnography Test. For the second variable, quantitative data were obtained from the EHR (BETP, 2017; Kiekkas et al., 2016). The clinical questions to be answered using data analysis were:
- Q1: Does the implementation of the AHA Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care impact nurses’ knowledge of capnography, compared to current practice, among ICU nurses in an acute care hospital in Southern New Jersey over four weeks?
- Q2: Does the implementation of the American Heart Association’s AHA Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care for Emergency Care impact the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest in an acute care hospital in Southern New Jersey over four weeks?
Data analysis methods are critical to quasi-experimental projects in that they assist in determining any effects that the independent variable may have on the dependent variable(s). In this project, first the difference between pre-test and post-test values was determined to show whether change happened during the intervention. The use of two measurement points – before and after the intervention – for both variables implied the need for a comparative test. Knowledge scores were calculated based on the percentage of correct responses with a range from 0% to 100%, thus they were considered interval data. To compare pre-intervention to post-intervention knowledge scores, paired t-tests were used for the total knowledge scores on all 30 items combined and on each NKCT subscale. Four subscales were compared between pre- and post-intervention scores.
For the second variable, the rates of ROSC after each resuscitation effort, according to the code situations’ datasheets were calculated and input into the Statistical Package for Social Sciences (SPSS) processing software. Each record was coded as “yes” or “no” based on whether ROSC was achieved. The percentage of health records with the rate of ROSC in the comparative (four weeks before the intervention) and post-implementation (four weeks after the intervention) groups were compared using a Fisher’s exact test. It was essential to present the data in the form of rates since the initial numbers of ROSC may not have represented the overall rate of numbers achieved during the two periods of data collection. The level of statistical significance for the project was set at p = 0.05, which is a standard level used in many studies in nursing (Cronin et al., 2014).
The use of specific statistical tools, such as SPSS, ensured the correctness of data analysis while also supporting the analysis process. The chosen data analysis procedure also related to the purpose of the project as it explored the possible relationship between nurses’ knowledge of capnography and their use of this tool during resuscitation in great depth. Further, it determined the impact of the implementation of capnography protocols on ROSC rates.
Potential Bias and Mitigation
There was a potential risk of bias in the stages of data collection and analysis. Taking the test in a controlled environment was important to reduce the risk of bias (Price et al., 2017). If nurses were to take an online test, they would have been able to search for additional materials, thus showing a higher level of knowledge than they possessed. Therefore, the proposed procedure was benefited the quality of the findings. Each test was completed in the intensive care unit, on paper and marked with the nurse’s identification number to prevent bias in quantitative data results. It is vital to note that nurses’ names did not appear on paper, nor were their names or other identifying information collected, lowering the risk of a privacy breach.
Another point of bias was the calculation of changes before and after the intervention. The use of the ROSC rates as a result of CPR before and after the educational intervention was necessary to mitigate this risk as the unit may have vastly different numbers of code situations, thus producing varying results. However, the chosen setting had a history of a high number of CPR performed in the unit, thus lowering the impact of this concern on the project.
Ethical Considerations
The present project involved human subjects, and it was particularly important to protect their rights and conduct the project in an ethical way (Sanjari, Bahramnezhad, Fomani, Shoghi, & Cheraghi, 2014; Zyphur & Pierides, 2017). The key ethical issues related to the project were the confidentiality and privacy of personal information provided by the participants and the disruption of nurses’ workflow during the project. Both problems mentioned above could violate the principles of the Belmont Report, specifically justice, beneficence, and respect for person, since they might cause harm to the nurses and their patients (National Commission for the Protection of Human Subjects of Biomedical, & Behavioral Research, 1979).
To address these issues, the project was modeled in a way that minimized workflow disruptions. For instance, testing took place outside of the nurses’ shifts, and data collection were conducted from the EHR without disturbing patients or staff. Additionally, measures to protect data privacy and confidentiality were applied. Personal information about the participants was stored safely on a password-protected device and will be destroyed after one year by deleting electronic documents and shredding paper documentation. Identifying information, including names and e-mail addresses, were replaced with identification numbers during data collection and analysis. No contact with patients was made throughout the project, so they experienced no risk of harm.
Institutional Review Board approval to conduct the project was received (see Appendix A), which meant the nurses fully understood their rights of participation as well as their ability to refuse the use of information for the project. Prior to IRB approval from GCU and the clinical site IRB, Collaborative Institutional Training Initiative (CITI) training education was completed to ensure that the principles of the Belmont Report were present in the project methodology, design, and population selection. No potential conflicts of interest were identified since the investigator was not connected to the hospital or nurses who participated in the project. As the project may be published in scholarly journals, precautions will be taken to protect subjects’ privacy and confidentiality at the publication stage. The documents shown to third parties will be checked to ensure the absence of identifying information, and the publication will only reveal the findings and not contain any identification numbers.
The data shared by the institution and the nurse participants were stored securely on a password-protected computer, and the participants’ numbers were used instead of their names during data collection and analysis. The data will be held for one year following the end of the project and will be destroyed per the policy of the project site. Explanations concerning the purpose, methodology, and design of the project were presented in their entirety to the nurses, and e-mail verification was used to solidify understanding. These precautions were in accordance with the European University Institute (EUI, 2019) guide on data protection practices, and they helped to ensure that the participants’ rights were preserved throughout the duration of the project. Additionally, it is important to note that no contact with patients was made during the project, and thus patients’ health and well-being were affected by the project in any way.
Limitations
While the project was carefully designed to provide high-quality information on the problem and avoid bias, there were still several limitations related to its methodology. Firstly, the sample size of the project was smaller than in other quantitative studies in nursing (Cronin et al., 2014). Additionally, the focus was on an intensive care unit, limiting the number of nurses in the sample. Enhancing the scope of the project would not have helped to achieve project goals because most other units have a lower frequency of cardiac arrest and would thus provide incomplete data. Hence, the chosen sample size was the best option given the geographic location of the project.
Another limitation was the facility under investigation had only two portable capnography monitors available, which meant that nurses would be able to use capnography in two simultaneous code stations. However, it was reported by the unit’s representatives, that it was rare for more than two codes to happen at the same time, so this limitation presented a low risk to the project. If a third code were to occur, the project’s results could be influenced, and any possible instances were recorded to ensure transparency. In preparation of the COVID-19 pandemic, it was recommended that the educators or leadership discuss with staff the safety measures utilized during codes at the height of the COVID-19 pandemic. Examples included minimizing staff in the patients’ rooms to essential personnel, keeping the code cart outside of the room, and having the pharmacist hand medications to the nurse in the room.
Finally, the length of the project, which collected information for two periods each spanning over four weeks, was another limitation. While the number of resuscitations in the ICU may be higher than some other units, four weeks is still a relatively short duration for collecting a substantial number of instances to calculate rates that would show improvement between pre- and postintervention numbers. Nevertheless, tests, such as Fisher’s exact test, were developed to present reliable findings even in small samples (Connelly, 2016).
Summary
Chapter 3 has described the methods utilized to conduct the investigation and answer the following clinical questions:
- Q1: Does the implementation of the AHA Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care impact nurses’ knowledge of capnography, compared to current practice, among ICU nurses in an acute care hospital in Southern New Jersey over four weeks?
- Q2: Does the implementation of the American Heart Association’s Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care for Emergency Care impact the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest in an acute care hospital in Southern New Jersey over four weeks?
The quantitative methodology was used as it was considered the best fit for the project’s purpose because it provided the objective data needed to establish the relationship between the variables (Barnham, 2015; Cronin et al., 2014). Additionally, the quasi-experimental design of the project was tailored to the needs of the investigation because it focused on establishing the level of change and the relationship between the three variables (Curtis et al., 2016). The data collection procedures that involved conducting surveys of nurses’ knowledge about the appropriate use of capnography through NKCT and data gathering from the EHR provided adequate measurements of the variables was presented. Baseline data were extracted four weeks before the program started, and all information was de-identified to ensure participants’ privacy. Then, four weeks after the project, the data were collected again to provide a second dataset for comparison.
Descriptive statistics were used to organize data and enrich the findings. Paired t-tests and Fisher’s exact test were applied to draw conclusions from the data sources and establish connections between the variables (Price et al., 2017). The sequence of procedures chosen for the project helped to answer to the clinical questions and fulfill the purpose of the project in evaluating and improving clinical practice.
Chapter 4 presents the results of the data analysis, which was performed after the project was completed. Results are presented in narrative and visual formats. Chapter 5 presents the interpretation of the results. Additionally, the implications of the findings for theory, practice, and the future are discussed. Chapter 5 ends with recommendations for future projects and practice.
Data Analysis and Results
This study was conducted to understand the relationship between nurses’ adoption of capnography, clinical uncertainty, and the lack of knowledge to use capnography assess ROSC in a clinical setting. It was not known if or to what degree the implementation of the American Heart Association’s (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Emergency Care would impact nurses’ knowledge of capnography and increase the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest when compared to current practice in urban New Jersey. It was also not clear whether the nurses’ lack of knowledge impeded the application of capnography in clinical settings (Kiekkaset al., 2016).
In efforts to address this problem, this quantitative, quasi-experimental project was implemented to educate nurses from a 20-bed ICU at a 240-bed acute care hospital in New Jersey on the use of capnography and the AHA guidelines to assess ROSC during CPR. It was then determined if knowledge improved after education when compared to before education using the NKCT (see Appendix B). Patient health records were examined for a comparative group (n = 12) and an implementation group (n = 10) to see if ROSC rate in the ICU increased or decreased during CPR after the intervention.
The data were collected to analyze two clinical questions:
- Q1: Does the implementation of the AHA Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care impact nurses’ knowledge of capnography, compared to current practice, among ICU nurses in an acute care hospital in Southern New Jersey over four weeks?
- Q2: Does the implementation of the AHA Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care for Emergency Care impact the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest in an acute care hospital in Southern New Jersey over four weeks?
The following sections offer information on the descriptive data for the two population samples. Data analysis procedures are described in-depth. Then, the results of the project and a summary of the findings are presented.
Descriptive Data
Demographic data were gathered for the nurse sample and the patient sample. Table 1 displays the demographic characteristics of the 13 nurses who participated in the project. As shown, the majority were staff nurses (92.3%). All were female (100%), and the most common response for highest degree was Bachelor of Nursing Science (BSN) (76.9%). Over half (53.8%) were between 31 to 40 years old. Time as a nurse was most often reported to be six to 11 years (30.8%).
Table 1: RN Sample Demographics (n = 13)
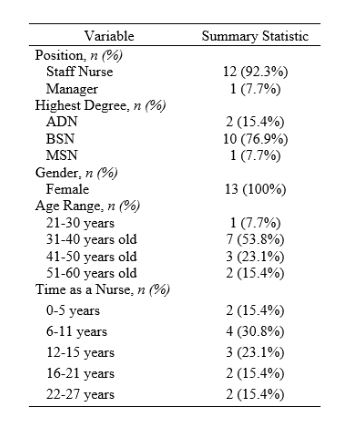
The patient information collected included age, gender, and ethnicity. Demographics for the comparative and implementation patient groups are displayed in Table 2. The average age was 68.8 years for the comparative group, and 69.5 years for the implementation group. There was an equal distribution of males and females for both groups with 50% of each gender. The majority of patients reported their ethnicity as White: 83.3% for the comparative group and 80% for the implementation group.
Table 2: Patient Demographics
Data Analysis Procedures
The purpose of this quantitative, quasi-experimental project was to determine if and to what degree the implementation the American Heart Association’s (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care would impact nurses’ knowledge of capnography and the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest, when compared to current practice, in an acute care hospital in Southern New Jersey over four weeks. The independent variable for this project was the educational intervention based on the American Heart Association’s (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care (Panchal et al., 2019). The dependent variables were nurses’ knowledge of capnography as measured by the Nurses’ Knowledge of Capnography Test (Kiekkas et al., 2016), and ROSC, which was obtained from the facility Code Blue datasheet, specifically for the documentation of end-tidal CO2 monitoring during CPR. A 3-item Likert scale post-intervention survey on perception of knowledge and understanding capnography use given to nurses was obtained and hard-copy values were entered in the dataset. Data were entered in SPSS version 26 for analysis.
After data entry, knowledge items were combined to create new variables. These new variables included a total score and four subscale scores for the NKCT knowledge test. Subscale scores were computed as: [(number of correct responses/total items in the subscale x 100)]. Total scores were computed as: [(total number of correct responses out of the total number of items answered x 100)]. These calculations offered an easy-to-interpret value with a range from 0 to 100 with higher scores reflecting better knowledge.
Preliminary analyses, including frequency counts, box-plot analysis, and Shapiro-Wilks’ tests, were conducted to ensure the data did not contain outliers and to check for normality of the distribution of scores. To determine if knowledge increased, a series of paired t-tests were conducted on each NKCT subscale score and on the total NKCT knowledge score at pre- vs. post-educational intervention. To examine use of capnography, a Fisher’s exact test was conducted. These results were used to determine if the ROSC rate for the four-week implementation was significantly different than ROSC rate in the four-week comparative group. Descriptive statistics (n, %) were computed for the 3-item post intervention nurse survey. Alpha was set to.05 for analyses.
As noted above, such tests as the frequency counts, box-plot analysis, and Shapiro-Wilks’ tests were completed to ensure the normality of gathered data and minimize the risk of misrepresenting the results of the sample (Watson, 2015). Paired t-tests for the measurement of the NKCT score changes were chosen as they are often used to determine the differences between two sets of data taken from two different points in time (Watson, 2015). This implies that two populations with two samples are used and the dependent variables are compared to detect a significant change. Finally, a Fisher’s exact test for measuring the changes in ROSC rates was selected due to its ability to show significant results even for small samples (Connelly, 2016). This calculation is utilized when one has two nominal variables and wants to see whether the proportions of the variable (ROSC rate) are different from the values of another variable (nurse’ education) (Connelly, 2016).
Results
The results are presented according to the two primary dependent variables. The first dependent variable was nurses’ knowledge as measured by the NKCT at pre- and post-educational intervention. The second variable presented is ROSC rates for patients with a CPR code for the comparative and implementation groups. For the nurses’ sample, the paired t-tests were completed using the data collected from the NKCT. These calculations aimed at showing the significance of changes before and after the educational intervention. Furthermore, a small survey was completed by nurses at the end of the investigation to assess their response to the intervention. The results of this survey were tested with descriptive statistics (n, %). A Fisher’s exact test was used for patients to show how the ROSC rate differed in patient samples before and after the educational program. The results of these tests were used to answer the two clinical questions and are presented below.
Nurses’ knowledge. The results of the paired t-tests showed a statistically significant increase in all subscales and total knowledge scores from pre- to post-educational intervention. Table 2 displays the mean (SD) for subscales and total knowledge scores in addition to t-values and p-values for the paired t-tests. As shown, there was a statistically significant improvement in knowledge scores on all four of the NKCT subscales. For the total score using all 30 items, there was a statistically significant improvement in knowledge scores from pre (M = 67.4, SD = 5.8) to post (M = 92.1, SD = 6.2), t(12) = -10.65, p =.000.
Table 3: NKCT Paired t-Test Results
ROSC rates. The percentage of ROSCs in the comparative group was 25% (3 out of 12 patients), and this slightly decreased in the implementation group to 20% (2 out of 10 patients). A Fisher’s exact test showed this to be a non-significant difference with a p-value of.999. Figure 1 displays ROSCs for the comparative and implementation groups.
Post-intervention survey for nurses. The 3-item Likert scale survey was analyzed using descriptive statistics (n, %). The results are displayed in Table 4 and reveal that nurses’ perceptions were positive regarding the education as the majority (84.7%) reported “agree” or “strongly agree” on improved knowledge, understanding of use during CPR, and understanding of documentation.
Table 4: Post-Intervention Nurse Survey Results (N=13)
Summary
The purpose of this quantitative, quasi-experimental project was to determine if and to what degree the implementation of the AHA Guidelines for Cardiopulmonary Resuscitation would impact nurses’ knowledge of capnography and the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest when compared to current practice at a 20-bed ICU in an acute care hospital in Southern New Jersey over four weeks. Two clinical questions were answered using a quantitative, quasi-experimental design involving a sample of 13 nurses and 22 patients.
The first question asked: Does the implementation of the impact nurses’ knowledge regarding the use of (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care impact nurses’ knowledge of capnography, when compared to current practice among ICU nurses in an acute care hospital in Southern New Jersey over four weeks? The dependent variable to answer this question was the score on the NKCT test. The NKCT test was given to nurses before and after an educational intervention. The test included four subscales with specific areas of knowledge and then a total knowledge score. The results of the paired t-tests showed a significant increase in all subscales and total knowledge scores from pre- to post-educational intervention for the 13 nurses who participated in the project. For the total score across all 30 items, there was a statistically significant improvement from pre (M = 67.4, SD = 5.8) to post (M = 92.1, SD = 6.2), t(12) = -10.65, p =.000. These results suggested that the educational intervention had a statistically and clinically significant impact on nurses’ knowledge of capnography.
The second clinical question asked: Does the implementation of the American Heart Association’s (AHA) Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care for Emergency Care impact the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest in an acute care hospital in Southern New Jersey over four weeks? For the second clinical question, the dependent variable was ROSC rate. There was a comparative group (n = 12) and implementation group (n = 10), and a total of 22 patient records were reviewed. The percentage of ROSCs in the comparative group was 25% (3 out of 12 patients) and this slightly decreased in the implementation group to 20% (2 out of 10 patients). A Fisher’s exact test showed this to be a non-significant difference with a p-value of.999. The ROSC rate slightly reduced, which suggested a further need to improve the nurse response and documentation for patients experiencing cardiac arrest.
Finally, a 3-item post-intervention survey on nurses’ perceptions was performed to collect some feedback about nurses’ opinions about the educational intervention. The results revealed positive perceptions regarding the education as the majority (84.7%) of nurses reported “agree” or “strongly agree” on improved knowledge, understanding of use during CPR, and understanding of documentation. Notably, almost half of respondents “strongly agreed” that the intervention was helpful in teaching them about capnography.
The next chapter offers a summary and conclusions for the study based on these results. Findings are compared with previous studies’ findings on capnography use for CPR codes. The theoretical and practical implications are also discussed as well as the recommendations for future research and practice and application in clinical settings.
Summary, Conclusions, and Recommendations
Nurses’ knowledge pertaining to clinical devices used for monitoring, assessing, and treating patients with heart conditions is an important factor for achieving quality of patient care and organizational effectiveness (Cook & Harrop-Griffiths, 2019). Studies conducted by Linet al. (2017), Novais and Moreira (2015), and Pantazopoulos et al. (2015) alluded to the lack of knowledge among nurses in using capnography as recommended by the Advanced Cardiac Life Support (ACLS) to capture pertinent information about a patient’s end-tidal carbon dioxide (ETCO2) condition. These researchers found that such low awareness of this approach presents uncertainties and poor clinical monitoring practices. The purpose of this quantitative, quasi-experimental project was to determine if and to what degree the implementation of the AHA Guidelines for Cardiopulmonary Resuscitation would impact nurses’ knowledge of capnography and the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest when compared to current practice at a 20-bed ICU in an acute care hospital in Southern New Jersey over four weeks.
In examining the level of knowledge, this project focused on ascertaining the strength, vulnerabilities, and weaknesses specific to the nursing awareness about the use of capnography during cardiopulmonary resuscitation. Additionally, the author of the project examined the correlation between such knowledge and the use of capnography during CPR and determined if any connections existed between nursing knowledge and nurses’ use of capnography in the cases of CPR. This objective was to provide some understanding of the differences in the nursing knowledge in using capnography during cardiopulmonary resuscitation and offer new information so as to achieve efficiency in the adoption of capnography for managing patients with CPR. The outcomes of this project included a positive clinical nursing practice change that clinical managers could use to moderate nurses’ adoption of clinical devices in the hospital setting and improve clinical outcomes for patients. Chapter 5 presents the summary of the project, discusses the findings and their implications for theory and practice, and provides recommendations for future quality improvement projects and academic research.
Summary of the Project
The goal of this project was to determine to what degree the implementation of capnography during cardiopulmonary resuscitation (CPR), when compared to the current practice, would impact nurses, and increase use of capnography during CPR for adult ICU patients. This project involved a quantitative investigation of the effect of a nursing education program on improving knowledge about capnography and how that can impact the use of capnography during CPR for ICU patients. The project used a paired sample of nurses for the dependent variable of capnography knowledge and two independent patient record sample groups for the dependent variable of capnography use for CPR codes.
The clinical questions for this project were as follows:
- Q1: Does the implementation of the AHA Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care impact nurses’ knowledge of capnography, compared to current practice, among ICU nurses in an acute care hospital in Southern New Jersey over four weeks?
- Q2: Does the implementation of the American Heart Association’s Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care for Emergency Care impact the rate of return of spontaneous circulation (ROSC) in ICU patients experiencing cardiac arrest in an acute care hospital in Southern New Jersey over four weeks?
In answering these clinical questions, the study addressed one of the main issues regarding the limited use of capnography in emergency and non-emergency situations as well as nurses’ lack of knowledge about capnography use. Given that capnography provides an extensive assessment of a patient’s well-being that is useful not only in emergency care but also in the day-to-day monitoring of patients, it provides medical personnel with a better understanding of a patient’s health status. The interpretation of waveforms can serve more purposes than that of the measurement of ETCO2 alone. This project addressed the importance of the use of this monitoring tool and nurses’ knowledge about the use and clinical value of capnography.
Two theoretical frameworks were used to guide the interpretation of the findings and these included Tanner’s model of clinical judgment and Lewin’s change theory. According to the former approach, a nurse must go through four phases of clinical judgment to deliver informed high-quality care, noticing, interpreting, responding, and judging. Tanner (2006) emphasized that all phases are influenced by nurses’ unit culture and their knowledge of both practical and theoretical sides of patient care. This theory enriched the present project by supporting the idea that nursing education can positively impact the choice to implement certain procedures (capnography) into nurses’ routines.
The second theoretical framework was Lewin’s change model, which outlines the process of change and separates it into three distinct steps – unfreezing, changing, and refreezing (Lewin, 1951). The discussion of the first and second steps was the most valuable for this project as Lewin (1951) argued that participants who are not well prepared for change are highly resistant to it. The introduction of the educational program included in the present project was a part of unfreezing because it provided a new framework of thought to nurses and outlined the possibilities of change, which the project hopes to prove, and led to practice evolution.
Summary of Findings and Conclusion
The first key finding of this project revealed increases in nurses’ knowledge for all four of the NKCT subscales, and three of the four scales showed statistically significant improvement with p-values of.000 for all three subscales. The subscale that did not show significant improvement was “Conditions affecting capnography waveform” which did show improvement, but the p-value was.154 (Kiekkas et al., 2016, p. 43). For the overall score across all 30 items, there was a statistically significant improvement in knowledge scores overall from pre (M = 72.1, SD = 9.) to post (M = 91.8, SD = 6.0), t(18) = -8.13, p =.000.
The education on capnography was based on the framework designed by Kiekkas et al. (2016), who chose to include 30 items into the quantitative instrument. The items contained statements about capnography, which nurses had to determine to be either correct or false. The findings of the present project supported the use of the authors’ 30-item instrument to measure nurses’ change in capnography-related knowledge. These results were used to assess the effectiveness of the learning program and demonstrated that teaching nurses about capnography and AHA guidelines on capnography was effective.
As found during pre-test examinations, nurses’ knowledge of capnography for use during resuscitation was limited. This finding was consistent with the article by Kaminska et al. (2017), who showed the same dearth of information being spread among emergency medical staff. Although the number of similar projects and research studies that examine the use of capnography by nurses during CPR was incredibly low, the DPI project’s outcomes are similar to one other work on the same topic. Mohammed et al. (2019) looked at the influence of an educational program on nurses’ knowledge of capnography in critical care units. They showed an increase in nurses’ total knowledge of the practice, and the present project’s findings agree with that conclusion. While the researchers did not employ the tool developed by Kiekkas et al. (2016), their conclusions were consistent with the DPI project in that they showed a clear improvement in nurses’ understanding of capnography after the learning intervention.
The second key finding of this project was that the percentage of records with capnography use in the pre-intervention was 10% (1 out of 10 patients), and this remained the same for the post-intervention period with 10% receiving capnography (1 out of 10 patients). A Fisher’s exact test showed this to be a non-statistically significant increase with a p-value of.999. As can be seen, the education program implemented at the beginning of the DPI project influenced nurses’ use of capnography. Capnography use for CPR has been studied for decades, but the results of its use are still not solidified in many organizations’ guidelines (Dioso, 2014). Nevertheless, the project’s findings strengthen previous research by such authors as Pantazopoulos et al. (2015), Merckx et al. (1992), Kodali and Urman (2014), Kalenda (1978), Hartmann et al. (2014), Elola et al. (2019), and others. Early works by Kalenda (1978) and Merckx et al. (1992) outlined the benefits of using capnography during resuscitation, the main one being the ability to continuously monitor pulmonary perfusion to guide the cardiac massage and adjust the performance in real time. As the training program for the present project was based on a similar idea, the findings of increasing in the ROSC rates imply that the effectiveness of capnography had been recognized by nurses who participated in the project.
Implications
The findings of this project have implications for theory, practice, and the future. For theory, the findings were supported the models by Tanner and Lewin, which served as the theoretical frameworks of the project. In terms of practice, the findings showed support for the education of capnography to increase its use and positively impact CPR code protocol for ICU patients. Findings also have implications for future investigators of quality improvement projects.
Theoretical implications
For this project, Tanner’s model of clinical judgment and Lewin’s change model were used as theoretical frameworks. Tanner’s framework claims that nursing culture in the unit and their knowledge of theoretical and practical concepts have a great impact on clinical judgments. These judgments are informed by nurses’ awareness as well as their environment when interpreting patient data and responding to their conclusions with specific actions (Tanner, 2006).
The findings from this project supported the ideas expressed in Tanner’s model of clinical judgment. The theoretical implication of the project’s outcomes was that nursing education has a great role in influencing healthcare decision-making, broadening nurses’ understanding of tools and devices they consider when performing routine or emergency procedures. Therefore, learning interventions on such subjects as capnography can change the way a whole unit approaches a situation when an informed clinical judgment is needed.
Lewin’s change model was also considered a basis for the project because the latter followed a philosophy of change. In his framework, Lewin (1951) distinguished three stages of a change initiative: unfreezing, changing, and refreezing. The theory also suggested that people are often reluctant to change and need to be prepared by the organization to embrace a new structure with learning and communication. This project adhered to the idea that resistance to change arises from the lack of unfreezing activities, including education.
The findings from this project supported the basic ideas of the change model. The theoretical implication of the findings is that the outcome of any intervention project depends on the amount of preparation that the change leader has made and the response of participants to unfreezing measures. At the basic level, the learning program about capnography laid a foundation for nurses to embrace this procedure and implement capnography use during CPR.
Practical implications
This project’s goal was geared toward improving CPR codes by increasing capnography use, which could help improve patient outcomes. According to one of the first articles noting the benefits of capnography for CPR, Kalenda (1978) stated that capnography allows the performance during CPR to be adjusted in real-time, which leads to the achievement of the maximal result – the highest chance of successful CPR. As Bullock et al. (2017) explained, the benefits of capnography during resuscitation were recognized by the American Heart Association (AHA) and the International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science, which updated their guidelines with these data to recommend capnography during CPR. Bullock et al. (2017) supported the idea that capnography has the ability to improve the quality of chest compressions, in turn, improving the chances of success in resuscitation. This project’s findings provide continued to support that capnography has many benefits for CPR and that the growing knowledge of nurses in the area is connected to wider use.
Future implications
This project offered an insight into capnography knowledge and capnography use. It outlined how an intervention can increase the use of capnography during CPR. This offers benefits within the healthcare industry because the project shows a potential way for an organization to introduce guidelines, such as the use of capnography during resuscitation, to nurses with the aim to implement change. The theoretical foundations of the project strengthen the strategy of the learning program and show that by addressing nurses’ lack of knowledge with targeted educational interventions, a unit culture can be influenced towards change. The findings revealed the effectiveness of knowledge-based interventions, while also showing that ways of assessing one’s understanding of such information exist.
Recommendations
Several recommendations could be made based on the outcome of this project. These included recommendations for future research, focusing on the theoretical significance of the findings. Recommendations for practice and application in clinical settings were also included for the unit under investigation and other potential healthcare providers.
Recommendations for future research
Although this project has a good theoretical foundation and a reliable quantitative methodology, the size, and the setting of it present some opportunities for improvement in future studies. First, the project analyzed results from a single unit in one hospital, which limited the transferability of the results to other hospitals. Notably, the chosen unit has a higher rate of resuscitations due to the emergency of patients’ cases. Therefore, the nurses working in this unit may have a different understanding or experience with the procedure and devices employed during CPR.
To combat this limitation, future projects should look at a wider range of participants, including nurses from different units and locations, acknowledging their work experience and specialization. Thus, the first three recommendations are to use a larger pool of participants, a wider range of different nurse specializations, and several geographical areas for exploration. The fourth recommendation is to develop a framework for controlling such variables as nurses’ learning outside of the training program to adjust for their personal interest in the topic. It is also possible to research whether some types of learning about capnography during CPR are more useful and successful than others in increasing the rate and correctness of capnography application.
Recommendations for practice
It is also recommended that healthcare providers receive education on the value of capnography use for ICU CPR codes. As demonstrated in the review of literature, such training is important because it broadens nurses’ scope of knowledge and provides new information on the use of capnography. As noted by Bullock et al. (2017), Chicote et al. (2019), and Aramendi et al. (2017), capnography use leads to an accurate feedback on ventilation during CPR, high accuracy and sensitivity to changes during the procedure, and the increased quality of chest compressions. In turn, the improvements in resuscitation increase the rate of successful CPR and positive patient outcomes, contributing to the quality of care.
The training program presented in the project can be implemented not only in the ICU but in other settings as well – all locations where CPR is performed can benefit from educating nurses on the benefits of capnography. This recommendation is crucial because out-of-hospital cardiac arrests and similar cases in other units of hospitals require nurses to make informed, but quick, judgments regarding treatment. Lui et al. (2016) found that capnography use can benefit out-of-hospital settings as well, underlining the crucial role of understanding capnography to improve resuscitation. Nurses, hospital administration members, and quality improvement project managers can benefit from learning about the results of this project to assess their staff’s knowledge of capnography and their preparedness for a change project to improve practice quality.
This DPI project sought to improve knowledge about capnography and improve the use of capnography during CPR for ICU patients. Lewin’s change theory and Tanner’s model of clinical judgment were used as theoretical frameworks to guide the project. These principles guided the overall process of the project, including the intervention and interpretation of the results. The analyses of the project revealed that such findings suggested that nurses’ knowledge of capnography increased after the learning intervention and that the tool developed by Kiekkas et al. (2016) helps investigators to appraise nurses’ understanding of the topic.
In this project, the increased awareness of the benefits related to capnography led to an insignificant increase in ROSC rates after CPR in the unit. This outcome implies that, while nurses’ education and unit culture plays a great role in nurses’ clinical judgment, other factors may also influence the outcome of CPR. In efforts to improve patient outcomes, this study supports capnography education to improve knowledge for nurses in ICU units. Recommendations for future research and improvement projects include increasing the sample size, diversifying the participants, and introducing a control measure to account for nurses’ individual interest in acquiring knowledge on the topic.
References
Alessandri, G., Zuffianò, A., & Perinelli, E. (2017). Evaluating intervention programs with a pretest-posttest design: A structural equation modeling approach. Frontiers in Psychology, 8(223), 1-12.
Ali, Z., & Bhaskar, S. B. (2016). Basic statistical tools in research and data analysis. Indian Journal of Anaesthesia, 60(9), 662-669.
Aramendi, E., Elola, A., Alonso, E., Irusta, U., Daya, M., Russell, J. K.,… Sterz, F. (2017). Feasibility of the capnogram to monitor ventilation rate during cardiopulmonary resuscitation. Resuscitation, 110, 162-168.
Aramendi, E., Lu, Y., Chang, M., Elola, A., Irusta, U., Owens, P., & Idris, A. (2018). A novel technique to assess the quality of ventilation during pre-hospital cardiopulmonary resuscitation. Resuscitation, 132, 41-46.
Austin, Z., & Sutton, J. (2014). Qualitative research: Getting started. The Canadian Journal of Hospital Pharmacy, 67(6), 436-440.
Barnham, C. (2015). Quantitative and qualitative research: Perceptual foundations. International Journal of Market Research, 57(6), 837-854.
Bullock, A., Dodington, J. M., Donoghue, A. J., & Langhan, M. L. (2017). Capnography use during intubation and cardiopulmonary resuscitation in the pediatric emergency department. Pediatric Emergency Care, 33(7), 457-461.
Bureau of EMS, Trauma, & Preparedness. (2017). Procedures: End-tidal carbon dioxide monitoring. Web.
Burnes, B. (2004). Kurt Lewin and the planned approach to change: A re‐appraisal. Journal of Management Studies, 41(6), 977-1002.
Burnes, B., & Bargal, D. (2017). Kurt Lewin: 70 years on. Journal of Change Management, 17(2), 91-100.
Campbell, C. M. (2017). An inside view: The utility of quantitative observation in understanding college educational experiences. Journal of College Student Development, 58(2), 290-299.
Carlisle, H. (2015). Promoting the use of capnography in acute care settings: An evidence-based practice project. Journal of Perianesthesia Nursing, 30(3), 201-208.
Center for Innovation in Research and Teaching. (2013a). Quantitative approaches. Web.
Center for Innovation in Research and Teaching. (2013b). When to use quantitative methods. Web.
Cereceda-Sánchez, F. J., & Molina-Mula, J. (2017). Capnography as a tool to detect metabolic changes in patients cared for in the emergency setting. Revista Latino-Americana de Enfermagem, 25, 1-10.
Chhajed, P. N., Gehrer, S., Pandey, K. V., Vaidya, P. J., Leuppi, J. D., Tamm, M., & Strobel, W. (2016). Utility of transcutaneous capnography for optimization of non-invasive ventilation pressures. Journal of Clinical & Diagnostic Research, 10(9), OC06-OC09.
Chicote, B., Aramendi, E., Irusta, U., Owens, P., Daya, M., & Idris, A. (2019). Value of capnography to predict defibrillation success in out-of-hospital cardiac arrest. Resuscitation, 138, 74-81.
Connelly, L. M. (2016). Fisher’s exact test. MedSurg Nursing, 25(1), 58-60.
Conway, A., Collins, P., Chang, K., Mafeld, S., Sutherland, J., & Fingleton, J. (2019). Sequence analysis of capnography waveform abnormalities during nurse-administered procedural sedation and analgesia in the cardiac catheterization laboratory. Scientific Reports, 9(1).
Cook, T., & Harrop-Griffiths, W. (2019). Capnography prevents avoidable deaths. BMJ, 364(l439), 1-9.
Cronin, P., Coughlan, M., & Smith, V. (2014). Understanding nursing and healthcare research. New York, NY: Sage.
Cummings, S., Bridgman, T., & Brown, K. G. (2016). Unfreezing change as three steps: Rethinking Kurt Lewin’s legacy for change management. Human Relations, 69(1), 33-60.
Darocha, T., Kosiński, S., Jarosz, A., Podsiadło, P., Ziętkiewicz, M., Sanak, T., … Drwiła, R. (2017). Should capnography be used as a guide for choosing a ventilation strategy in circulatory shock caused by severe hypothermia? Observational case-series study. Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine, 25(1), 15.
de Caen, A., & Maconochie, I. (2018). EtCO2 measurement during pediatric cardiac arrest: Does the Emperor have no clothes? Resuscitation, 133, A1-A2.
Dioso, R. P. (2014). Compression-only cardiopulmonary resuscitation as an assessment tool for nursing students – an evaluative literature review. Malaysian Journal of Nursing, 6(1), 44-49.
Duckworth, R. L. (2017). How to read and interpret end-tidal capnography waveforms. Journal of Emergency Medical Services, 42(8). Web.
Edelson, D. P., Yuen, T. C., Mancini, M. E., Davis, D. P., Hunt, E. A., Miller, J. A., & Abella, B. S. (2014). Hospital cardiac arrest resuscitation practice in the United States: A nationally representative survey. Journal of Hospital Medicine, 9(6), 353-357.
Elola, A., Aramendi, E., Irusta, U., Alonso, E., Lu, Y., Chang, M.P., … Idris, A.H. (2019). Capnography: A support tool for the detection of return of spontaneous circulation in out-of-hospital cardiac arrest. Resuscitation, 142, 153-161.
European University Institute. (2019). Guide on good data protection practice in research. Web.
Fawcett, J. (2016). Applying conceptual models of nursing: Quality improvement, research, and practice. New York, NY: Springer.
Fawcett, J., & Ellenbecker, C. H. (2015). A proposed conceptual model of nursing and population health. Nursing Outlook, 63(3), 288-298.
Flanagan, S. M., Greenfield, S., Coad, J., & Neilson, S. (2015). An exploration of the data collection methods utilised with children, teenagers, and young people (CTYPs). BMC Research Notes, 8(1), 61.
Flick, U. (2018). An introduction to qualitative research. New York, NY: Sage Publications Limited.
Gong, Y., Lu, Y., Zhang, L., Zhang, H., & Li, Y. (2015). Predict defibrillation outcome using stepping increment of pointcare plot for out-of-hospital ventricular fibrillation cardiac arrest. Biomed Research International, 2015, 493472.
Gravenstein, J. S., Jaffe, M. B., Gravenstein, N., & Paulus, D. A. (Eds.). (2011). Capnography (2nd ed.). Cambridge, UK: Cambridge University Press.
Green, J., & Thorogood, N. (2018). Qualitative methods for health research. New York, NY: Sage.
Gunnell, M. (2016). Research methodologies: A comparison of quantitative, qualitative, and mixed methods. Web.
Guo, H., Kurokawa, T., Takahata, M., Hong, W., Katsuyama, Y., Luo, F., … Gong, J.P. (2016). Quantitative observation of electric potential distribution of brittle polyelectrolyte hydrogels using microelectrode technique. Macromolecules, 49(8), 3100-3108.
Gutiérrez, J. J., Leturiondo, M., de Gauna, S.R., Ruiz, J. M., Leturiondo, L. A., González-Otero, D. M., … Daya, M. (2018). Enhancing ventilation detection during cardiopulmonary resuscitation by filtering chest compression artifact from the capnography waveform. PLoS ONE, 13(8), e0201565.
Haines, L. E. (2017). Continuous-waveform capnography: A crucial tool for ED clinicians. American Nurse Today, 12(1). Web.
Hamrick, J. T., Hamrick, J. L., Bhalala, U., Armstrong, J. S., Lee, J. H., Kulikowicz, E., … Shaffner, D. H. (2017). End-tidal CO2–guided chest compression delivery improves survival in a neonatal asphyxial cardiac arrest model. Pediatric Critical Care Medicine, 18(11), 575-584.
Harper, C. (2005). Capnography: Clinical aspects. Journal of the Royal Society of Medicine, 98(4), 184-185.
Hartmann, S. M., Farris, R. W., Di Gennaro, J. L., Roberts, J. S. (2015). Systematic review and meta-analysis of end-tidal carbon dioxide values associated with return of spontaneous circulation during cardiopulmonary resuscitation. Journal of Intensive Care, 30, 426–35.
Hassankhani, H., Aghdam, A. M., Rahmani, A., & Mohammadpoorfard, Z. (2015). The relationship between learning motivation and self-efficacy among nursing students. Research and Development in Medical Education, 4(1), 97-101.
Heale, R., & Twycross, A. (2015). Validity and reliability in quantitative studies. Evidence-Based Nursing, 18(3), 66-67.
Heradstveit, B. E., & Heltne, J. K. (2014). PQRST–A unique aide-memoire for capnography interpretation during cardiac arrest. Resuscitation, 85(11), 1619-1620.
Hussain, S. T., Lei, S., Akram, T., Haider, M. J., Hussain, S. H., & Ali, M. (2018). Kurt Lewin’s change model: A critical review of the role of leadership and employee involvement in organizational change. Journal of Innovation & Knowledge, 3(3), 123-127.
Ingham-Broomfield, R. (2014). A nurses’ guide to quantitative research. The Australian Journal of Advanced Nursing, 32(2), 32-38.
Israel, C. W. (2014). Mechanisms of sudden cardiac death. Indian Heart Journal, 66(1), 10-17.
Izrailtyan, I., Qiu, J., Overdyk, F. J., Ersion, M., Gan, T. J. (2018). Risk factors for cardiopulmonary and respiratory arrest in medical and surgical hospital patients on opioid analgesics and sedatives. PLoS ONE, 13, e0194553.
Jaffe, M. B. (2017). Using the features of the time and volumetric capnogram for classification and prediction. Journal of Clinical Monitoring and Computing, 31(1), 19-41.
Jones, T. (2016). Outcome measurement in nursing: Imperatives, ideals, history, and challenges. The Online Journal of Issues in Nursing, 21(2), 1-11.
Jooste, R., Roberts, F., Mndolo, S., Mabedi, D., Chikumbanje, S., Whitaker, D., & O’Sullivan, E. (2018). Global capnography project (GCAP): Implementation of capnography in Malawi – an international anaesthesia quality improvement project. Anesthesia, 74(2), 158-166.
Kalenda, Z. (1978). The capnogram as a guide to the efficacy of cardiac massage. Resuscitation, 6(4), 259-263.
Kalmar, A.F., Allaert, S., Pletinckx, P., Maes, J.W., Heerman, J., Vos, J.J., … Scheeren, T.W.L. (2018). Phenylephrine increases cardiac output by raising cardiac preload in patients with anesthesia induced hypotension. Journal of Clinical Monitoring and Computing, 1(1), 1-8.
Kaminska, H., Wieczorek, W., Dabrowski, M., Nadolny, K., & Smereka, J. (2018). Knowledge and attitudes of paramedics toward the usage of capnography as a ventilation monitoring tool during resuscitation. The American Journal of Emergency Medicine, 36(6), 1116-1117.
Katz-Buonincontro, J., & Anderson, R. (2018). How do we get from good to great? The need for better observation studies of creativity in education (Opinion article). Frontiers in Psychology, 9, 2342.
Kerslake, I., & Kelly, F. (2017). Uses of capnography in the critical care unit. BJA Education, 17(5), 178-183.
Kiekkas, P., Stefanopoulos, N., Konstantinou, E., Bakalis, N., & Aretha, D. (2016). Development and psychometric evaluation of an instrument for the assessment of nurses’ knowledge on capnography. Collegian, 23(1), 39-46.
Kodali, B. S. (2013). Capnography outside the operating rooms. Anesthesiology: The Journal of the American Society of Anesthesiologists, 118(1), 192-201.
Kodali, B. S., & Urman, R. D. (2014). Capnography during cardiopulmonary resuscitation: Current evidence and future directions. Journal of Emergencies, Trauma, and Shock, 7(4), 332-340.
Kuisma, M., Salo, A., Puolakka, J., Nurmi, J., Kirves, H., Väyrynen, T., & Boyd, J. (2017). Delayed return of spontaneous circulation (the Lazarus phenomenon) after cessation of out-of-hospital cardiopulmonary resuscitation. Resuscitation, 118, 107-111.
Lampe, J. (2017). Improved ventilation monitoring during CPR. Resuscitation, 110, A3-A4.
Langham, M. L., Li, F. Y., & Lichtor, J. L. (2016). Respiratory depression detected by capnography among children in the postanesthesia care unit: A cross-sectional study. Pediatric Anaesthesia, 10, 1010-1017.
Langham, M. L., Li, F. Y., & Lichtor, J. L. (2017). The impact of capnography monitoring among children and adolescents in the postanesthesia care unit: A randomized controlled trial. Pediatric Anaesthsia, 27, 385-393.
Langhan, M. L., Shabanova, V., Li, F. Y., Bernstein, S. L., & Shapiro, E. D. (2015). A randomized controlled trial of capnography during sedation in a pediatric emergency setting. The American Journal of Emergency Medicine, 33(1), 25-30.
Leppink, J., O’Sullivan, P., & Winston, K. (2016). On variation and uncertainty. Perspectives on Medical Education, 5(4), 231-234.
Leturiondo, M., Ruiz de Gauna, S., Julio Gutiérrez, J., M. González-Otero, D., M. Ruiz, J., A. Leturiondo, L., & Saiz, P. (2019). Waveform capnography for monitoring ventilation during cardiopulmonary resuscitation: The problem of chest compression artifact. Cardiac Diseases in 21St Century. IntechOpen. Web.
Leturiondo, M., Ruiz de Gauna, S., Ruiz, J. M., Julio Gutiérrez, J., Leturiondo, L. A., González-Otero, D. M., … Daya, M. (2018). Influence of chest compression artefact on capnogram-based ventilation detection during out-of-hospital cardiopulmonary resuscitation. Resuscitation, 124, 63–68.
Lewin, K. (1951). Field theory in social science. New York, NY: Harper & Row.
Lin, K. J., Singer, D. E., Glynn, R. J., Murphy, S. N., Lii, J., & Schneeweiss, S. (2018). Identifying patients with high data completeness to improve validity of comparative effectiveness research in electronic health records data. Clinical Pharmacology & Therapeutics, 103(5), 899-905.
Lin, T.Y., Fang, Y.F., Huang, S.H., Wang, T.Y., Kuo, C.H., Wu, H.T., … Lo, Y.L. (2017). Capnography monitoring the hypoventilation during the induction of bronchoscopic sedation: A randomized controlled trial. Scientific Reports, 7(1), 8685-8687.
Lin, Y., Guerguerian, A., Laussen, P., & Trbovich, P. (2015). Heuristic evaluation of data integration and visualization software used for continuous monitoring to support intensive care: A bedside nurses perspective. Journal of Nursing Care, 4(300), 2167-1168.
Link, M. S., Berkow, L. C., Kudenchuk, P. J., Halperin, H. R., Hess, E. P., Moitra, V. K., … Donnino, M. W. (2015). Adult advanced cardiovascular life support. Circulation, 132, 444-64.
Long, B., Koyfman, A., & Vivirito, M. A. (2017). Capnography in the emergency department: A review of uses, waveforms, and limitations. Journal of Emergency Medicine, 53, 829-842.
Lui, C. T., Poon, K. M., & Tsui, K. L. (2016). Abrupt rise of end tidal carbon dioxide level was a specific but non-sensitive marker of return of spontaneous circulation in patient with out-of-hospital cardiac arrest. Resuscitation, 104, 53-58.
Mader, T. J., Coute, R. A., Kellogg, A. R., & Harris, J. L. (2014). Coronary perfusion pressure response to high-dose intraosseous versus standard-dose intravenous epinephrine administration after prolonged cardiac arrest. Open Journal of Emergency Medicine, 2(1), 1-7.
Martínez-Mesa, J., González-Chica, D. A., Bastos, J. L., Bonamigo, R. R., & Duquia, R. P. (2014). Sample size: How many participants do I need in my research? Anais Brasileiros de Dermatologia, 89(4), 609-615.
Merckx, P., Lambert, Y., Cantineau, J., & Duvaidestin, P. (1992). Effect of capnography on resuscitation efforts during CPR. Resuscitation, 24(2), 189.
Mohamed, W. K. (2019). Effect of teaching program on nurses’ knowledge and practice regarding measuring end-carbon dioxide by capnography at critical care units. Assiut Scientific Nursing Journal, 7(18), 145-153.
Morse, J. M. (2017). Analyzing and conceptualizing the theoretical foundations of nursing. New York, NY: Springer.
Nassar, B. S., & Schmidt, G. A. (2016). Capnography during critical illness. Chest, 149(2), 576-585.
Nassar, B., & Kerber, R. (2017). Improving CPR performance. Chest, 152(5), 1061-1069.
National Commission for the Protection of Human Subjects of Biomedical, & Behavioral Research. (1979). The Belmont report: Ethical principles and guidelines for the protection of human subjects of research. Web.
Nelson, D. (2018). Quantitative observation: Definition and examples. Web.
Novais, P. M., & Moreira, M. M. (2015). Capnography: A feasible tool in clinical and experimental settings. Respiratory Care, 60(11), 1711-1713.
Panchal, A. R., Berg, K. M., Hirsch, K. G., Kudenchuk, P. J., Del Rios, M., Cabañas, J. G.,… Donnino, M. W. (2019). 2019 American Heart Association focused update on advanced cardiovascular life support: Use of advanced airways, vasopressors, and extracorporeal cardiopulmonary resuscitation during cardiac arrest: An update to the American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation, 140(24), e881-e894.
Pantazopoulos, C., Xanthos, T., Pantazopoulos, I., Papalois, A., Kouskouni, E., & Iacovidou, N. (2015). A review of carbon dioxide monitoring during adult cardiopulmonary resuscitation. Heart, Lung and Circulation, 24(11), 1053-1061.
Price, P. C., Jhangiani, R. S., Chiang, I. A., Leighton, D., & Cuttler, C. (2017). Research methods in psychology (3rd ed.). New York, NY: The Saylor Foundation.
Ristagno, G., Mauri, T., Cesana, G., Li, Y., Finzi, A., Fumagalli, F., … Latini, R. (2015). Amplitude spectrum area to guide defibrillation: A validation on 1617 patients with ventricular fibrillation. Circulation, 131(5), 478–487.
Ruiz de Gauna, S., Leturiondo, M., Gutiérrez, J., Ruiz, J., González-Otero, D., Russell, J., & Daya, M. (2018). Enhancement of capnogram waveform in the presence of chest compression artefact during cardiopulmonary resuscitation. Resuscitation, 133, 53-58.
Sahyoun, C., Siliciano, C., & Kessler, D. (2018). Use of capnography and cardiopulmonary resuscitation feedback devices among prehospital advanced life support providers. Pediatric Emergency Care, 1-8.
Salen, P., O’Connor, R., Sierzenski, P., Passarello, B., Pancu, D., Melanson, S.,… Heller, M. (2001). Can cardiac sonography and capnography be used independently and in combination to predict resuscitation outcomes? Academic Emergency Medicine, 8(6), 610-615.
Sandroni, C., De Santis, P., & D’Arrigo, S. (2018). Capnography during cardiac arrest. Resuscitation, 132, 73-77.
Sanjari, M., Bahramnezhad, F., Fomani, F. K., Shoghi, M., & Cheraghi, M. A. (2014). Ethical challenges of researchers in qualitative studies: The necessity to develop a specific guideline. Journal of Medical Ethics and History of Medicine, 7, 14. Web.
Saunders, R., Struya, M., Pollock, R., Mestek, M., & Lightdale, J. (2017). Patient safety during procedural sedation using capnography monitoring: A systemic review and meta-analysis. BMJ Open, 7, e013402.
Sheak, K.R., Wiebe, D.J., Leary, M., Babaeizadeh, S., Yuen, T.C., Zive, D., … Abella, B.S. (2015). Quantitative relationship between end-tidal carbon dioxide and CPR quality during both in-hospital and out-of-hospital cardiac arrest. Resuscitation, 89, 149-154.
Soar, J., Nolan, J. P., Böttiger, B. W., Perkins, G. D., Lott, C., Carli, P., … Adult Advanced Life Support Section Collaborators. (2015). Adult advanced life support. Resuscitation, 95, 100-147.
Stites, M., Surprise, J., McNiel, J., Northrop, D., & De Ruyter, M. (2017). Continuous capnography reduces the incidence of opioid-induced respiratory rescue by hospital rapid resuscitation team. Journal of Patient Safety, 1-10.
Subramani, Y., Singh, M., Wong, J., Kushida, C., Mahotra, A., & Chung, F. (2017). Understanding phenotypes of obstructive sleep apnea: applications in anesthesia, surgery, and perioperative medicine. Anesthesia Analgesia, 124, 179-191.
Tanner, C. A. (2006). Thinking like a nurse: A research-based model of clinical judgment in nursing. Journal of Nursing Education, 45(6), 204-211.
Tobi, K. U., & Amadasun, F. E. (2015). Cardio-pulmonary resuscitation in the intensive care unit: An experience from a tertiary hospital in Sub-Saharan Africa. Nigerian Medical Journal: Journal of the Nigeria Medical Association, 56(2), 132-137.
Turle, S., Sherren, P., Nicholson, S., Callaghan, T., & Shepherd, S. (2015). Availability and use of capnography for in-hospital cardiac arrests in the United Kingdom. Resuscitation, 94, 80-84.
Udod, S., & Wagner, J. (2018). Common change theories and application to different nursing situations. In J. Wagner (Ed.), Leadership and Influencing Change in Nursing (pp. 155-173). Regina, Canada: University of Regina Press.
Valente, M. J., & MacKinnon, D. P. (2017). Comparing models of change to estimate the mediated effect in the pretest–posttest control group design. Structural Equation Modeling: A Multidisciplinary Journal, 24(3), 428-450.
Venkatesh, H., & Keating, E. (2017). BET 1: Can the value of end tidal CO2 prognosticate ROSC in patients coming into emergency department with an out-of-hospital cardiac arrest (OOHCA)? Emergency Medicine Journal, 34(3), 187-189.
Watson, R. (2015). Quantitative research. Nursing Standard, 29(31), 44-48.
Whitaker, D., & Benson, J. (2016). Capnography standards for outside the operating room. Current Opinion in Anaesthesiology, 29(4), 485-492.
Wright, S. (2017). The case for procedural capnography. Web.
Wright, S. A. (2017). The case for procedural capnography [DNP project]. Capella University, Minneapolis, MN. Web.
Yen, P. Y., Kelley, M., Lopetegui, M., Rosado, A. L., Migliore, E. M., Chipps, E. M., & Buck, J. (2016). Understanding and visualizing multitasking and task switching activities: A time motion study to capture nursing workflow. In AMIA Annual Symposium Proceedings (pp. 1264-1273). New York, NY: American Medical Informatics Association.
Zito, A., Berardinelli, A., Butler, R., Morrison, S., & Albert, N. (2019). Association of end-tidal carbon dioxide monitoring with nurses’ confidence in patient readiness for postanesthesia discharge. Journal of Perianesthesia Nursing.
Zyphur, M. J., & Pierides, D. C. (2017). Is quantitative research ethical? Tools for ethically practicing, evaluating, and using quantitative research. Journal of Business Ethics, 143(1), 1-16.
Appendix A
IRB Approval Letter
Appendix B
NKCT Items
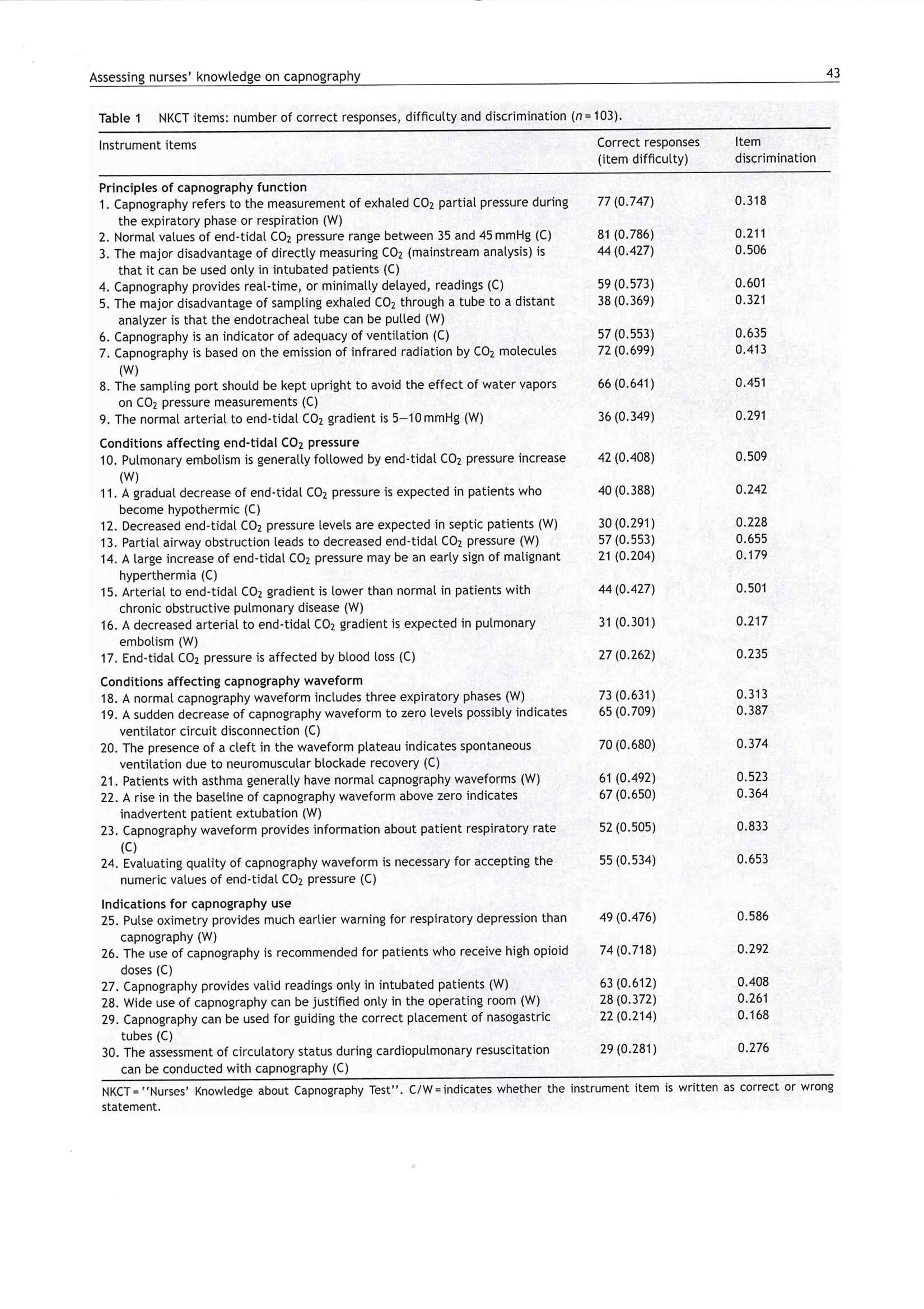
Appendix C
Permission to Use the Tool
