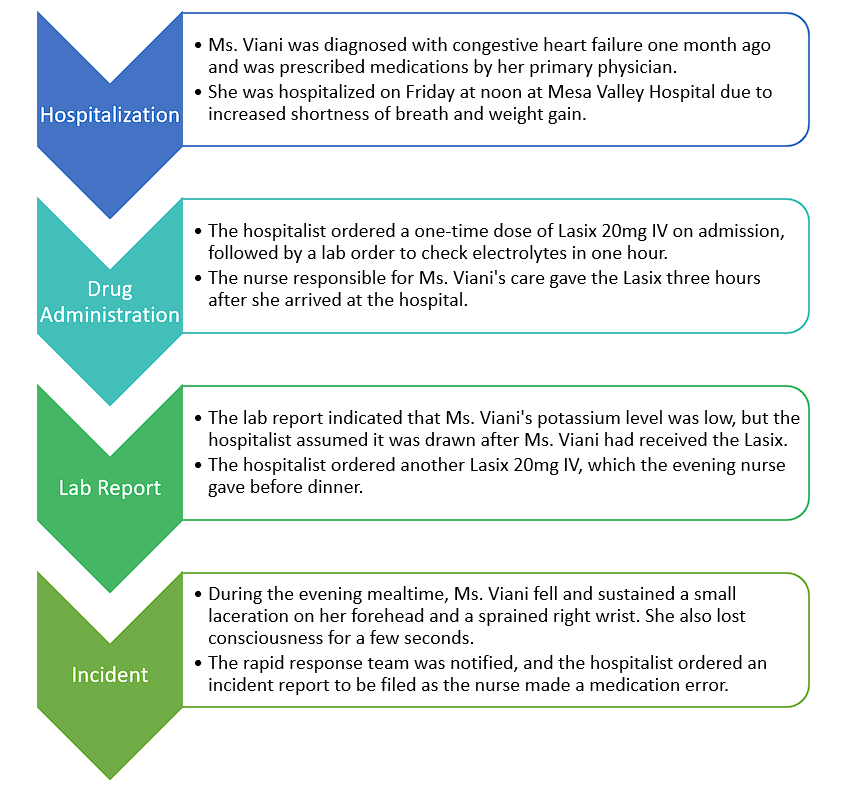
Root Cause Analysis: Timeline
Figure 1 below is a Root Cause Analysis flowchart with summaries of events, processes, and staff involved. The timeline suggests that the medical error occurred due to delays in administering the Lasix and misinterpretation of the lab results, which may have been due to communication gaps between the staff involved.
Root Cause Analysis: Factors
On the basis of the flowchart of events, there are two contributing factors and one causal factor that led to the medical error. Firstly, the two contributing factors include inadequate staffing levels and communication gaps. For the former, the nurse responsible for Ms. Viani’s care was busy and gave the Lasix three hours after she arrived at the hospital. This delay may have been due to a high workload caused by inadequate staffing levels. For the communication gaps, the nurse did not inform the hospitalist that the Lasix had been given late, which could have helped the hospitalist make a more informed decision about ordering another dose. This suggests that there may be communication gaps between the staff involved in Ms. Viani’s care.
In the case of the causal factor, the lack of standardized processes for medication administration can be noted. The delayed administration of Lasix may have been due to a lack of standardized processes for medication administration at the hospital. If there were clear protocols in place for administering medications, the nurse might have been able to give the Lasix on time, which may have prevented Ms. Viani’s condition from worsening. Thus, these contributing and causal factors suggest that improvements in staffing levels, communication protocols, and standardized medication administration processes could help prevent similar medical errors in the future.
Patient Safety Strategies: Recommendation
The evidence-based patient safety improvement strategy is to implement a standardized medication administration protocol that emphasizes the timely administration of medications and clear communication between healthcare providers. The measure is based on the contributing and causal factors identified in the Root Cause Analysis. Patients and families can play an important role in this strategy by being active participants in their own care (Carayon et al., 2020). They can ask questions about their medications and treatment plans, inform their healthcare providers about their medical history and any medications they are taking, and report any concerns they have about their care (Carayon et al., 2020). Patients and families can be involved in the development of the medication administration protocol by providing feedback on their experiences and suggesting ways to improve the process.
In addition to a standardized medication administration protocol, other patient safety strategies that can be implemented include regular training and education for healthcare providers on communication skills, teamwork, and patient safety culture. The hospital can conduct regular patient safety assessments and involve patients and families in the assessment process (Franck & O’Brien, 2019). The purpose is to identify areas for improvement and develop strategies to address them.
Patient Safety Strategies: Measurement
Several measures could be used to measure the effectiveness of the patient safety improvement strategy of implementing a standardized medication administration protocol. Firstly, a measurement of the timely administration of medications must be established. A primary measure of success could be the percentage of medications administered within a specified timeframe, such as 30 minutes before or after the scheduled time (Franck & O’Brien, 2019). Data on medication administration times should be collected and analyzed regularly to determine if improvements are being made.
Secondly, communication between healthcare providers can be a useful data source. Another measure of success could be the frequency and quality of communication between healthcare providers. This could be measured through staff surveys, patient satisfaction surveys, and incident reporting systems. Thirdly, the success of the patient safety improvement strategy should be measured by improvements in patient outcomes, such as reduced incidence of falls, adverse drug events, and hospital-acquired infections. Patient data, including readmission rates and length of hospital stay, should be tracked and analyzed over time to determine if the patient safety improvement strategy is leading to improved outcomes (Franck & O’Brien, 2019). In addition to these measures, regular staff training and education sessions, incident reporting and analysis, and patient safety assessments can provide valuable feedback and help determine whether the patient safety improvement strategy is achieving its intended goals.
Details
The necessary details to disclose the error to the patient and family, based on state and federal reporting requirements and the results of the root cause analysis, can be outlined as follows. The first detail is a clear explanation of the medication error that occurred, which involved the delayed administration of Lasix upon admission and the subsequent administration of an additional dose by the evening nurse. These actions may have contributed to Ms. Viani’s fall and the injuries she sustained (Hart et al., 2020). The second detail involves sharing the contributing factors that led to the error, such as inadequate staffing levels, communication gaps between healthcare providers, and the lack of standardized processes for medication administration. The third detail requires providing information on the consequences of the error, including Ms. Viani’s fall, the laceration on her forehead, the sprained right wrist, and the brief loss of consciousness. It is essential to ensure that the patient and family understand the relationship between the medication error and these outcomes.
The fourth detail pertains to discussing the immediate steps taken after the incident, such as notifying the rapid response team and filing an incident report. In addition, it is important to explain any medical interventions provided to address Ms. Viani’s injuries and monitor her condition (Hart et al., 2020). The fifth detail involves sharing the hospital’s plan to implement a standardized medication administration protocol, improve communication between healthcare providers, and address staffing levels to prevent similar errors in the future, emphasizing the hospital’s commitment to patient safety and continuous improvement.
The sixth detail is to encourage the patient and family to be active participants in their own care and to provide feedback on their experiences, explaining how their input will be valuable in the development and implementation of the patient safety improvement strategy. Lastly, as the seventh detail, it is crucial to offer a sincere apology for the error and the harm caused to Ms. Viani while expressing empathy and understanding for the distress and inconvenience the error may have caused the patient and family (Hart et al., 2020). This approach ensures that the disclosure of the error is comprehensive, transparent, and professional, fostering trust and collaboration between the healthcare providers, the patient, and the family.
Method and Preparation
A structured and empathetic approach should be adopted to effectively disclose these details to the patient and family. The method of disclosure should involve a face-to-face meeting with the patient and family, including the healthcare providers directly involved in the patient’s care, a representative from hospital administration, and, if appropriate, a patient advocate. Before the disclosure, thorough preparation is necessary. The staff should receive training in open and honest communication, disclosure techniques, and empathy to ensure a professional and compassionate approach (Kim & Lee, 2020). They should be well-informed about the incident, RCA results, and planned patient safety improvement strategy to address any questions or concerns the patient and family might have.
It is essential to schedule the meeting at a convenient time for the patient and family, ensuring privacy and sufficient time for discussion. Prior to the meeting, the patient and family should be informed that an important discussion regarding the patient’s care will take place without providing specific details about the error. This approach allows them to mentally prepare for the conversation and encourages their active participation (Kim & Lee, 2020). During the meeting, the healthcare providers should disclose the details sequentially, beginning with a clear explanation of the error, followed by contributing factors, patient impact, and the steps taken to address the incident. The disclosure should then focus on the patient safety improvement strategy and the importance of patient and family involvement and conclude with an apology and expression of empathy (Kim & Lee, 2020). By following this method and adequately preparing the staff, patient, and family, the disclosure process can be more effective, transparent, and compassionate, fostering trust and collaboration between all parties involved.
Reporting
When reporting the RCA and corrective action plan to accrediting or regulatory agencies, specific elements need to be shared to ensure transparency and compliance. Firstly, a comprehensive description of the medication error should be provided, encompassing the sequence of events that led to the delayed administration of Lasix and the subsequent administration of an additional dose (JCI, 2021). Second, it is important to disclose the underlying factors found in the RCA, such as low staffing levels, a lack of established procedures for administering medications, and communication breakdowns among healthcare workers.
Thirdly, the immediate steps taken to address the incident should be described, such as involving the rapid response team, filing an incident report, and providing appropriate medical interventions for the patient’s injuries. Fourthly, the corrective action plan should be outlined, which includes the patient safety improvement strategy focusing on implementing a standardized medication administration protocol, enhancing communication between healthcare providers, and addressing staffing levels (JCI, 2021). Lastly, the measures that will be used to evaluate the effectiveness of the corrective action plan should be explained, such as timely medication administration, improved communication, and patient outcomes (JCI, 2021). Reporting these elements ensures transparency and demonstrates the commitment of the healthcare organization to improve patient safety and prevent similar errors in the future.
References
Carayon, P., Wooldridge, A., Hoonakker, P., Hundt, A. S., & Kelly, M. M. (2020). SEIPS 3.0: Human-centered design of the patient journey for patient safety. Applied Ergonomics, 84, 103033. Web.
Franck, L. S., & O’Brien, K. (2019). The evolution of family-centered care: From supporting parent-delivered interventions to a model of family integrated care. Birth Defects Research, 111(15), 1044-1059. Web.
Hart, W. M., Doerr, P., Qian, Y., & McNaull, P. M. (2020). What constitutes effective team communication after an error? AMA Journal of Ethics, 22(4), 298-304. Web.
JCI. (2021). Joint Commission International Accreditation Standards for Hospitals [PDF document]. Web.
Kim, Y., & Lee, H. (2020). Nurses’ experiences with disclosure of patient safety incidents: A qualitative study. Risk Management and Healthcare Policy, 13, 453-464. Web.
