Research Question
The population of interest is African Americans with type 2 diabetes. The intervention is early detection of neuropathy in African-Americans with type 2 diabetes to prevent the development of the diabetic foot. The desired outcome is the prevention of the development of neuropathy to ensure that African-Americans with type 2 diabetes do not face the need to take additional medication or even go through an amputation.
PICO: Will early detection of neuropathy in African Americans with type 2 diabetes reduce the development of diabetic foot ulcers when compared to those with late detection of neuropathy.
Hypothesis: African Americans with type 2 diabetes whose neuropathy is detected early are less likely to develop a diabetic foot ulcer.
Objective and Specific Aims
Since the population of African-Americans with type 2 diabetes is disproportionately affected by foot problems that can lead to amputation, the objective is to find ways to address this healthcare concern. Thus, the objective is to develop strategies that healthcare professionals can use to detect the development of neuropathy in patients with type 2 diabetes of African-American ethnicity since these individuals are disproportionately affected. The specific research question is: What specific approaches can healthcare professionals use to prevent neuropathy in this population? What are the risk factors of neuropathy in African-Americans with type 2 diabetes?
Introduction
Damage to or dysfunction of one or more nerves is known as neuropathy, and the common symptoms include pain, numbness, tingling, and weakness in the afflicted muscles. Neuropathies often begin in your hands and feet, but they can also affect other parts of your body (Zakin et al., 2019). An issue with the peripheral nervous system is indicated by neuropathy, often known as peripheral neuropathy. The network of nerves outside of one’s brain and spinal cord is known as your peripheral nervous system. One sort of nerve damage that can happen if a person has diabetes is diabetic neuropathy. Throughout the body, damaged nerves can result from high blood sugar or glucose. The nerves in the legs and feet are most frequently damaged by diabetic neuropathy (Zakin et al., 2019). Thus, neuropathy is a common complication for people with diabetes, and patients and healthcare providers should pay more attention to prevention and early detection.
Patients need to regularly examine their feet for discomfort, skin tears, calluses, blisters, and open sores. Additionally, they ought to wash your feet every day in warm water with soap. With a towel, gently pat dry the feet, being sure to dry in between the toes. After washing, they can apply a moisturizer to the foot skin to maintain moisture. However, these prevention methods can only be used if the person is educated on the prevention methods by their healthcare provider.
Diabetic neuropathy symptoms can range from numbness to discomfort in the hands, feet, and legs, depending on which nerves are impacted. Additionally, it may result in issues with the heart, blood vessels, digestive system, and urinary tract. Mild symptoms are present in some people. However, for some people, diabetic neuropathy can be quite painful and incapacitating. Up to 50% of patients with diabetes may develop diabetic neuropathy, a significant consequence of the disease (Zakin et al., 2019). But with constant blood sugar control and a healthy lifestyle, you may frequently prevent diabetic neuropathy or reduce its progression.
The focus of this research is on the population of African-Americans because this community is affected by diabetes complications disproportionately when compared to the majority of the population. African Americans are disproportionately affected by type 2 diabetes-related lower extremities problems (Bonner et al., 2019). Four hundred sixty-three million people worldwide are projected to have diabetes, and the figure is expected to climb to 578 million by 2030 and 700 million by 2045, according to the International Diabetes Federation 2020 (Bonner et al., 2019). Diabetes mellitus is a long-term glucose metabolism condition with substantial clinical repercussions. Microvascular endpoints and macrovascular endpoints are included in the multi-system consequences of diabetes. The diabetic foot ulcer, which, if left untreated, can result in infection, deep tissue necrosis, and limb amputation, is one of the most significant consequences of diabetes. Approximately 80% of lower extremity amputations caused by diabetes begin with a foot ulcer (Sharpe, 2020). Thus, foot-related complications are common among patients with diabetes, and individuals of African-American descent are disproportionately affected by this problem.
Research Methods
This review was completed using two databases that contain articles related to the medical field: Pubmed, Google Scholar, Cochrane, CINAHL, and Medline. This paper is based on the research of secondary data, which is information collected through empirical studies and published in peer-reviewed magazines. Secondary research is also referred to as desk research. There are essentially two types of research activities: primary research, in which the researcher sets out to find things, and secondary research, in which they examine what others have already done.
The type of study that is the target of this research is clinical research that engages patients who are routinely observed at a clinical facility or a quality improvement project. Quality Improvement (QI) initiatives or procedures, such as teaching evaluations and employee/patient satisfaction surveys, are systematic, data-driven efforts or processes intended to enhance clinical care, patient safety, health care operations, services, and programs. The goal of QI is to use the experience to find effective techniques, adopt those methods widely, and assess the changes that have been made and their immediate effects. Therefore, QI is a crucial component of effective clinical practice, where lessons learned are applied to improve patient care in the future, as well as healthcare operations, services, and programs at the institution where the QI activity is carried out. Implementing a procedure, for instance, to enhance the standard of patient care, as well as gathering and quickly evaluating data pertaining.
The type of participants is linked to the target population since this research focused primarily on the African-American population. According to the study, black adults had a considerably higher risk of developing diabetes than white ones did, with about 66 more cases of diabetes per 1,000 people (Sandriwala et al., 2018). The biggest distinction was between white women and black women. To ascertain how biological, local, psychosocial, socioeconomic, and behavioral risk factors affected diabetes incidence, the researchers performed statistical analyses. They discovered that the majority of the health discrepancy was caused by biological risk factors. Body mass index, waist size, fasting glucose levels, cholesterol, blood pressure, and lung function were some of the contributing variables (Domingos et al., 2021). Although to a lesser extent, differences in neighborhood, psychological, socioeconomic, and behavioral characteristics between blacks and whites were also associated with diabetes.
Desk research does not involve gathering data. Instead, as a user researcher conducting desk research, your job is to study the results of prior studies to get a comprehensive grasp of the subject. Desk research is used to describe secondary data or information that can be gathered without using the field (“Chapter 4,” n.d.). Most people assume it means published reports and statistics, which are unquestionably significant sources. The word is broadened in the context of this research to refer to all information sources that do not entail a field survey. This will undoubtedly involve looking through libraries and the internet, but it can also involve consulting with someone at a trade group or conducting expert interviews. Thus, the desk research that is the basis of this research study is a method that has a variety of definitions and primarily involves the use of internet resources and libraries to collect information on a given topic.
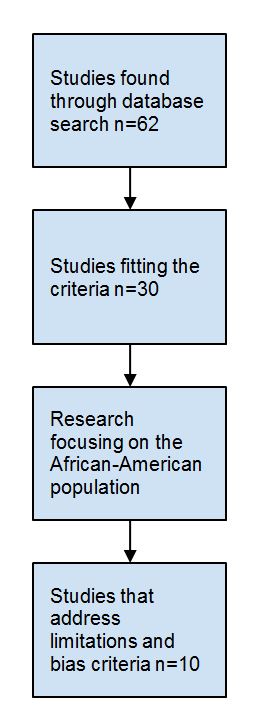
Over the course of this study, 62 articles were reviewed; however, only ten were selected to be a part of the final report. The researcher used keywords such as “foot ulcer,” “diabetes complications,” and “diabetes among Africa-Americans” to find the studies. The date of publication was limited to the years 2018-2022 to ensure that only the most recent data is taken into account. Additionally, the researcher examined the abstracts of the studies that fit the initial criteria to determine if the paper focuses on the aspects of diabetes that pertain to the African-American population. Below is the Prism diagram for this research that was developed by the author, displayed in Figure 1.
Methods of the Review
The reliability of qualitative research is frequently evaluated using four criteria: credibility, dependability, confirmability, and transferability. For the research to be credible, the technique must be carefully justified and explained. Dependability is the degree to which the study could be repeated under the same circumstances. Confirmability is the quality of having a distinct connection or relationship between the data and the conclusions. Transferability describes the ability to apply discoveries to a different setting, situation, or group.
The best suitable study design will frequently be chosen in response to the questions raised by the guideline. It is insufficient to base judgments about the reliability of the data just on the study type, such as believing randomized trials or systematic reviews to be more reliable than observational studies. Bias is used to describing elements that can consistently skew the study’s findings and observations away from reality. The possibility that elements of a study’s design or method would produce false results is known as its risk of bias. This may lead to the wastage of resources, the loss of possibilities for sensible solutions, or customer harm. A degree of methodological skill is required for risk of bias assessment, which can be carried out either by the guideline development group or by seasoned researchers as part of a commissioned evidence review.
Results of Individual Studies
As was mentioned in the “Methodology” part of this paper, in total, ten studies were selected for this paper. In the study by Sharpe (2020), the author reviewed the general characteristics of foot problems within the African-American population with diabetes. According to the author’s conclusions, numerous studies have been conducted regarding diabetic foot ulcer wound care, and the findings consistently emphasize the importance of prevention in the patient’s ability to manage their diabetes on their own. According to Bus and van Netten, prevention of such things gets minimal attention. Large datasets are reviewed for information about the ethnic minorities in recent self-management research in order to have a statistically significant sample size.
In a study by Bonner et al. (2019), the researchers found that education is the main factor in preventing foot ulcers that can further lead to amputation in the population in question. African Americans are disproportionately affected by type 2 diabetes-related lower extremities problems. Participants had less extended foot care knowledge than basic foot care knowledge when comparing the basic and extended foot care education means scores. This study also demonstrated that the presence of insurance had a significant impact on extended foot care knowledge. Regardless of education level or gender, there are significant disparities in how foot care information is transferred into actual foot self-care practices in an African American population with T2DM.
According to Domingos et al. (2021), The most crucial aspects of the care of patients with diabetes and amputations include family, economic, and employment environments, as well as aspects of the health care system. Since 44 percent of US, adults assist a family member or friend with managing a chronic condition, and another 9 percent are willing to start, family and friend support can actually be a valuable source of self-management support. This could theoretically explain our findings regarding the difference in the more favorable diet when comparing patients who live with or without a partner. When the participants were divided into groups according to their sex, significant differences (p0.05) were discovered in the questions “Specific Food” and “Foot care.” Significant differences (p 0.05) were found for the question “Specific Food” in relation to marital status. There were no differences between the groups with and without prior amputations. The authors were able to report using the SDSCA instrument that T2DM patients who had had emergency LLA displayed changes in self-care, notably for sex and marital status.
Liu et al. (2021) conducted a study between July and September 2020, in which patients with diabetic foot problems were gathered from three tertiary hospitals in China. Patients with a clinical diagnosis of diabetic foot problems, who were at least 18 years old, could communicate in Chinese as their first language, and who were open to discussing their treatment experiences were included. The in-person semi-structured interviews, which lasted 20 to 50 minutes and were audio-recorded, were conducted using an interview guide. We searched the transcripts for qualitative themes.
Sanz-Corbalán et al. (2018) want to demonstrate the earlier detection of the risk of developing diabetic foot ulcers (DFU) compared to routine clinical tests and to assess the utility of the sudomotor function test (SFT) as a clinical tool in the risk stratification system of diabetic patients. The average follow-up time was 42 months. After a median of 6.2 months, 60 patients (22.8%) experienced DFU. Based on the findings from the SWM and biothesiometer, ten of the patients in the no-risk group had DFU (Sanz-Corbalán et al., 2018). As a result, this method’s sensitivity was 83.33 percent, and its specificity was 50.47 percent (Sanz-Corbalán et al., 2018). All patients who experienced DFU were categorized into the appropriate risk group in accordance with the SFT results.
According to epidemiological research, drinking tea reduces your risk of developing type 2 diabetes and its complications (Meng et al., 2019). Through a number of potential mechanisms, including enhancing insulin action, reducing insulin resistance, activating the insulin signaling pathway, safeguarding islet -cells, scavenging free radicals, and reducing inflammation, experimental studies have shown that tea has protective effects against diabetes mellitus and its complications. Clinical investigations have also demonstrated the effectiveness of the tea intervention in individuals with diabetes mellitus and associated consequences (Callaghan et al., 2020). As a result, this article summarizes and discusses the effects of tea on diabetes mellitus and its complications based on the findings from epidemiological, experimental, and clinical studies, with a special focus on the role that tea plays in the prevention and management of diabetes mellitus and its complications.
Review Results
Limitations
As with any study, this research has its limitations. High rates of morbidity, disability, and mortality have been found to be connected with patients who have diabetic foot problems. Liu et al. (2021) aimed to explore the barriers patients with this disease faced, provide evidence to improve the effectiveness of medical services, discuss prevention and treatment strategies for future policymakers, and garner widespread attention from the Chinese society through the findings of qualitative interviews with patients with this disease.
This study relies on secondary data, which limits the ability of the researcher to determine all of the risk factors, barriers, and constraints. Additionally, there is no direct interaction with the subjects, and therefore, it is difficult to control the way each experiment in this study was conducted to ensure that all of the environments were appropriate.
Conclusions
In summary, Amputation-causing foot issues are disproportionately experienced by African Americans with type 2 diabetes. Patients and healthcare professionals should focus more on early detection and prevention of neuropathy in this population because it is a prevalent problem for diabetics. The affected muscles experience discomfort, numbness, tingling, and weakening as symptoms. Symptoms of diabetic neuropathy might include numbness and pain in the hands, feet, and legs. Lower extremity issues caused by type 2 diabetes disproportionately impact African Americans. A diabetic foot ulcer is the first complication in about 80% of lower extremity amputations brought on by diabetes. Biological risk factors were the primary cause of the health disparity. Waist circumference, fasting blood sugar, cholesterol, blood pressure, and lung function were all measured.
Implications for Practice
Based on this review, the practitioners can use patient education as one of the methods to address the complications of type 2 diabetes in the populations that are most vulnerable to the complications from this disease, which are African-Americans. Naturally, taking preventative measures won’t be the only option. It is clear that diabetes self-management education and training, which has been described as “the process of promoting the knowledge, skill, and capacity necessary for diabetic self-care,” will be necessary (Sharpee, 2020, 10). The importance of prevention lies in its ability to both save lives and lessen the pain and suffering of newly diagnosed diabetics. Many people with diabetes perceive their diagnosis as a prompt to begin losing the functionality of all physical functions, and they feel ignored because no one seems to have the time to talk to them instead of just giving them a brochure or website to look at.
Implications for Research
Since this study has found that prevention and patient education are the most effective methods for addressing foot problems in diabetic patients, more research should be done on the issue of effective ways of teaching patients to care for themselves and identifying the early signs of complications. Effective patient education can be used as a method for preventing neuropathy since it allows the patients to manage their self-care effectively.
Diabetes’ rising human and financial costs have alarmed people all around the world. The principal forms of the disease begin at younger and younger ages, in addition to the alarming rate of increase in the population affected. We now understand that diabetes affects a wide range of illnesses, including Alzheimer’s disease, cancer, liver failure, bone fractures, depression, and hearing loss, in addition to the usual acute metabolic and chronic vascular consequences. One-third of Medicare spending in the United States goes toward treating diabetic patients, and the percentage of CVD risk attributed to diabetes is growing. While diabetic problems may take decades to emerge, the disease’s origins may be in utero.
Thus the breadth of meaningful research extends across the life span, ranging from studies of how the in utero environment alters diabetes risk to improved understanding of the special needs of older patients with diabetes. Since the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) was established in 1950, we have seen huge progress in our ability to predict, classify, and treat diabetes and its complications as well as to prevent or delay type 2 diabetes. Landmark NIDDK-led clinical trials have demonstrated that glucose control can dramatically reduce diabetes complications, and lifestyle change producing modest weight loss, or the drug metformin, can substantially reduce the development of type 2 diabetes.
The National Institutes of Health (NIH) invests more than $1 billion annually in diabetes research in a difficult economic environment (Liu et al., 2019). About two-thirds of this sum goes to NIDDK, and we’re committed to making sure that these funds are allocated properly and in a way that balances competing demands. We need to find and utilize innovative pathways that will offer new targets and strategies for treating the illness while simultaneously addressing the most pressing practical problems concerning clinical management, prevention, and treatment of diabetes and its consequences. Under the direction of NIDDK, a new strategic plan for diabetes research was published last year with participation from over 100 scientists, numerous government agencies, and NIH components (Liu et al., 2019).
The plan outlines developments and possibilities in ten main areas as well as the need for resources and infrastructure. The fight against diabetes will require a variety of skills and knowledge, from behavioral and social sciences to molecular and cell biology. For this project to succeed, it is essential to develop and empower this human capital. This will enable multidisciplinary cooperation and the use of new technologies in diabetes research. We will briefly discuss our aims and activities for diabetes research here, directing readers to the Diabetes Research Strategic Plan (1) for a more thorough examination of the developments and prospects.
In order to enhance outcomes for those who have diabetes or are at risk of developing it, we must have a scientific staff that is both well-trained and diverse. The NIDDK supports training grants, fellowships, and career award mechanisms to provide opportunities for investigators at all phases of the career trajectory in order to ensure a pipeline of fresh, well-trained investigators in basic and clinical disciplines. Programs tailored to particular needs are added to these, such as our medical student research program in diabetes, which enables students to conduct research at one of our 17 NIDDK-funded Diabetes Research Centers under the supervision of an accomplished scientist; supplements to research and training grants to promote the recruitment of underrepresented minority scientists to diabetes research; and institutional career development programs to draw pediatricians.
References
Callaghan, B., Gallagher, G., Fridman, V., & Feldman, E. (2020). Diabetic neuropathy: What does the future hold? Diabetologia, 63(5), 891-897.
Chapter 4. (n.d.). Web.
Bonner, T., Guidry, J., & Jackson, Z. (2019). Association between foot care knowledge and practices among African Americans with type 2 diabetes: An exploratory pilot study. Journal of The National Medical Association, 111(3), 256-261.
Domingos, S., França, C., Tuleta, I., Barbosa, M., Bachi, A., Melo Neves, L. (2021). Self-care in type 2 diabetes patients with urgency lower limb amputation: The influence of sex, marital status, and previous amputations. Patient Preference and Adherence, 15, 1083-1090.
Liu, X., Chu, H., Zhao, J., Qiao, R., Liu, Y., & Li, N. et al. (2021). Exploring the barriers of patients with diabetic foot complications in China: A qualitative interview study. Annals of Translational Medicine, 9(9), 792-792.
Meng, J., Cao, S., Wei, X., Gan, R., Wang, Y., & Cai, S. (2019). Effects and mechanisms of tea for the prevention and management of fiabetes mellitus and diabetic complications: An updated review. Antioxidants, 8(6), 170.
Sadriwala, Q., Gedam, B., & Akhtar, M. (2018). Risk factors of amputation in diabetic foot infections. International Surgery Journal, 5(4), 1399.
Sanz-Corbalán, I., Lázaro-Martínez, J., García-Morales, E., Molines-Barroso, R., Álvaro-Afonso, F., & García-Álvarez, Y. (2018). Advantages of early diagnosis of diabetic neuropathy in the prevention of diabetic foot ulcers. Diabetes Research and Clinical Practice, 146, 148-154.
Sharpe, J. E. (2020). Eliminating the health disparity of the diabetic foot: A continuing public health crisis for African Americans and Latinos. International Journal of Diabetes And Clinical Research, 7(2), 10.
Zakin, E., Abrams, R., & Simpson, D. (2019). Diabetic neuropathy. Seminars in Neurology, 39(05), 560-569.
