Introduction
Obesity is one of the health risks that the current global population is facing. The world is undergoing both nutritional and epidemiological transitions that are marred by consistent nutritional deficiencies and marked by stunted growth, anemia, and mineral deficits in the body. In addition to nutritional deficiency diseases, cases of obesity have exponentially increased over the last two decades. Obesity is mainly associated with various metabolic abnormalities such as hyperglycemia, increased risk of coronary cardiac diseases, type 2 diabetes, asthma, hypertension, and certain types of cancers. However, different factors can be attributed to the rising cases of obesity. These factors are a sedentary lifestyle and overeating, all of which can be grouped as environmental factors. Extensively, genetic susceptibility determines the obesity status of a person. Another factor that is essential in the investigation of obesity is the biological development of organisms. Development is abstruse due to the fact that it is a characteristic of life that is tightly tied to both the genetics and environmental causes of obesity.
Excess weight is connected to both developmental biology and genetics in an extricate manner. By definition, development entails a gradual change in the size of an organism, shape, and function that translates from its genotypic potentials to its observable functioning mature systems. Therefore, the characteristics of an organism that is developed as it grows through life stages arise from hereditary factors. As such, the genes of obesity may be passed from a parent to the offspring in both humans and animals. Development also entails changes to specific body parts, such as the brain, skeletal muscles, and digestive system, among others. However, repetitive chemical alterations and those occurring over more than one lifetime are not part of the development process. With this explanation, it can be concluded that obesity is mostly an inherent disorder.
The interaction between genetic factors and development is impacted by the environment within which a life form operates. Physical and social factors can determine whether an organism will be obese. Examples of the factors that influence body-weight genes include prenatal and early life influences, poor nutritional choices, sedentary lifestyles, and little physical activity. Environmental factors generate the creation of an energy imbalance. Namely, the excess fat is stored in the body as adipose tissues. As much as hereditary factors play an essential role in determining obesity occurrence among organisms, external environmental factors also shape the development of genes. In essence, relationships between genetics, development, and environmental factors impact obesity occurrences. This article reviews the interactions that occur between genes, development, and environment in the molecular basis of obesity and excess weight among organisms.
Gene-Development Interaction in Obesity and Intervention
Heritability is a term explained within the purview of the interaction between genetics and biological development. Precisely, heritability is the portion of the observed variation in a particular trait that can be attributed to inherited genetic factors (Flores-Dorantes et al., 2020). In regards to heritability and obesity correlations, the BMI (Body mass index) scale was applied to assess differences in twins. Based on the observations obtained from analyzing more than 140,000 twins, heritability has been determined as ranging from 47 to 90 percent (Flores-Dorantes et al., 2020). Moreover, the studies concluded that the genetic factors’ contribution to BMI was higher in childhood than in adulthood. Based on the aforementioned data, it is inevitable that the effect of hereditary factors on obesity is more pronounced in the early stages of life.
Biological developments that facilitate changes in the deoxyribonucleic acid (DNA) strands form the basis of obesity categorization into different types depending on the genome. By applying gene-development interaction as a central point, obesity can be classified as monogenetic, polygenetic, or syndromic obesity. This article assesses only monogenetic and polygenetic obesities based on the gene-development interaction.
Genetics of Obesity
Monogenic Obesity
Monogenic obesity is the rarest form of the condition. It is caused by the mutations of one specific gene and can be described as having a severe early onset. Monogenic obesity is to be mentioned due to the fact that the gene that mutates is transmitted by an obese patent and develops in the offspring. The developments are generally facilitated by changes that the obesity gene undergoes to adapt to any possible intervention method aimed toward disorder control. As rare as this form of obesity is, approximately 7.3% of the condition initially occurs in one gene (Flores-Dorantes et al., 2020). Examples of genes associated with monogenetic obesity (see Appendix A) include leptin (LEP), leptin receptor (LEPR), proopiomelanocortin (POMC), preproconvertase 1 (PCSK1), single-minded 1 (SIM1), Melanocortin 4 receptor (MC4R), and tyrosine kinase receptor tropomyosin-related kinase B (TrkB) (Flores-Dorantes et al., 2020). Therefore, monogenetic obesity is a form of the condition that is caused by a single gene that undergoes certain mutations.
A variety of proteins participating in the development of the condition are a part of the leptin-melanocortin signaling pathway. The pathway is essential for balancing the energy in the hypothalamus through the management of energy intake and expenditure. Leptin activates proopiomelanocortin-expressing neurons, creating melanocortin peptides that have the function of binding the MC4R, which, in turn, manages the energy balance. Credible scientific studies have found that gene mutations in POMC and MC4R are linked to obesity due to an injury to the hypothalamus (Flores-Dorantes et al., 2020). As a result, one’s appetite increases on a biological level. Indeed, mutations in MC4R genes are prominent occurrences when it comes to monogenetic obesity. In humans, MC4Rs are highly susceptible to alterations. Additionally, mutations in the PCSK1 gene result in the misprocessing of melanocortin peptides, which ultimately lead to excess weight and malformations of glucose equipoise and adrenalin function (Flores-Dorantes et al., 2020). The transcription factor of the protein-coding gene SIM1 causes excess weight as a result of hypothalamus dysfunctions and the lessening of the paraventricular nucleus (PVN) in the same region of the brain. Based on the aforementioned information, it is inevitable that gene mutation correlates with obesity from a biological perspective.
Polygenetic Obesity
Polygenic obesity is another form of excess weight that correlates with genetic predispositions. The frequent occurrence of polygenetic obesity can be described as the polymorphism of different genes. Namely, polymorphism or single nucleotide variants (SNVs) are transformations of one nucleotide of the DNA order that develop in a large number of people (Flores-Dorantes et al., 2020). The discovery and analysis of this particular type of obesity have been achieved relatively recently due to the scientific development allowing innovative examinations to illustrate potential causes of excess weight. Frameworks, including molecular biology methods, have been applied to examine various forms of genes simultaneously at each developmental stage of a living organism. Moreover, the founding of scientific consortia, such as the UK Biobank or Genetic Investigation of Anthropometric Traits (GIANT) association, has facilitated advances in research. The phenomenon is attributed to an increase in sample studies that can be applied in genetic analysis. Various meta-analyses have been performed with the intention of identifying factors correlating with excess weight, such as body fat distribution in certain populations (Flores-Dorantes et al., 2020). Continuous research in genetics has, therefore provided insightful information on obesity classification.
Remarkably, several of the genes associated with excess weight are involved in neurogenesis, the development of the central nervous system (CNS), and elements such as appetite and food intake regulation. The genes determine the uptake of nutrients, energy inputs, and outputs that determine whether an organism is prone to obesity. Some of the hereditary units include MC4R, POMC, Fat Mass and Obesity-Associated Gene (FTO), Neurexin-3-alpha (NRXN3), and Niemann-Pick C1 (NPC1). (Flores-Dorantes et al., 2020). Moreover, specific genes that are related to synaptic function and neurotransmitter signaling include Neuronal Growth Regulator 1 (NEDR1), NRXN3, Cell Adhesion Molecule 2 (CADM2), and Glutamate Ionotropic Receptor Delta Type Subunit 1 (GRID1) (Flores-Dorantes et al., 2020). As mentioned prior, all the aforementioned genes morph, which illustrates how obesity occurs in relation to polymorphism.
Gene polymorphism has a mild effect on excess weight gain. However, risks increase depending on one’s genetics. Thus, the Genetic Risk Score (GRS) is applied to determine one’s susceptibility to obesity from an evidence-based perspective. The scale generates results that illustrate whether the risks are high, mild, or low. Furthermore, Khera et al. (2019) established a genome-wide polygenic score that encompasses a variety of potential genetic variables. As they are directly linked to obesity, the score examines the various factors and generates a quantitative measure portraying inherited susceptibility. Thus, the tool is applied to identify the likelihood of developing obesity on a genetic level.
It is crucial to point out that the occurrence of obesity has been linked to a multitude of genetic variants that directly or indirectly impact one’s weight. Current scientific progress allows individual risks to be determined, facilitating a relatively straightforward prediction of whether one will experience the condition. Therefore, strategies and interventions can be individualized for each person, yet more research is required for the framework to be validated by the entire scientific community. Nonetheless, the current state of obesity-related genetic studies is attributed to researchers who have identified each of the variants associated with excess weight. Thus, there is progress in regard to understanding obesity from the perspective of biological predispositions, the progression of the condition, and its manifestations.
Gene-Environment Interaction in Obesity and Intervention
Current research studies have reported that the increased likelihood of developing obesity correlates with the influence of environmental and physical factors on genes. Thus, it is essential to identify the connection between genes and the environment to determine how the phenomenon correlates with obesity. One interaction that has been described as a leading obesity cause is the obesity variants FTO and MC4R combined with certain lifestyle aspects (Flores-Dorantes et al., 2020). However, certain studies have highlighted that the implementation of intervention may ameliorate the effects. Thus, lifestyle changes such as implementing physical activities and strict adherence to the Mediterranean diet can regulate the obesity risk that is generated by FTO and MC4R variants (Flores-Dorantes et al., 2020). Moreover, gene variants have the potential to affect weight loss depending on the dietary practices of an individual. For example, FTO is associated with a change in appetite and abdominal fat distribution when exposed to a high or low protein diet. As a result, excessive weight is activated when the aforementioned genetic variants are combined with certain environmental factors, such as protein intake.
Several studies have explained that genetic factors are the major causative agents in the genetic basis for obesity. However, the researchers fail to explain the “missing heritability” in the study of obesity. An explanation of that particular phenomenon is associated with a variety of contrasting arguments. For instance, it has been found that BMI heritability stands between 47 to 90 percent. Applying an obesity hypothesis-free analysis while examining 941 gene variants, it has been illustrated that the gene variants only represented approximately 6% of the variance of BMI (Flores-Dorantes et al., 2020). As the variable correlates with a low rate of cases, the interest in researching further heritability decreases. The missing percentages can be explained by the influence of the environment over genetic factors.
The GRS is increasingly becoming more widely applied in determining the interaction between genes and the environment when it comes to obesity. GRS takes into account several genetic variants that can predict the outcomes and identify the variables that lead to weight excess. An example of influences impacting the obesity GRS is the consumption of sweetened drinks, which was determined through evidence generated from 30 obesity gene variations. (Flores-Dorantes et al., 2020). It is inevitable that genetics and environment interactions impact weight, but the list of variants that are susceptible to alterations due to external physical processes is relatively short. Another combination that results in weight changes is genetics and activity. The examination of 94 variants has led to conclusions illustrating that gene mutations were linked to one’s activity, sedentary lifestyle, and socioeconomic status (Flores-Dorantes et al., 2020). These results highlight that genes confer one’s susceptibility to obesity despite environmental modifications that can potentially minimize risks. Inarguably, adhering to a balanced diet and inducing a calorie deficit has been linked to an amelioration of obesity risks despite potential genetic predispositions.
Obesogenic Environment
Apart from the unidirectional interaction between genetic and external factors, it is vital to illustrate the relationship between the obesogenic environment and organisms interacting with it. A scientific experiment was performed to ascertain whether there is a relationship between the two elements. Results obtained from one specific study stated that dogs with obese owners were more likely to have excess weight as compared to those with lean owners (Flores-Dorantes et al., 2020). From the findings, obesogenic environmental conditions are to be considered as a phenomenon of the molecular basis for obesity and related disorders.
Major risk factors for obesity are frequently studied independently, yet their interaction is associated with an increase in susceptibility to developing obesity. Biologically, genes are an element of the natural world defined as the nucleotides that form human DNA. DNA differs, resulting in genetic variation and individual differences in traits (Rask-Anderson et al., 2017). On the other hand, the environment nurtures or modifies the attributes of an individual. Therefore, a person born lean can develop poor dietary habits that may lead to the accumulation of excess fat in the body, leading to the development of obesity.
Data that has been collected by scientists and organizations also confirm the interaction of genes and the environment as factors facilitating obesity. United Biobank, for instance, has sampled approximately 500,000 individuals from the United Kingdom (Flores-Dorantes et al., 2020). The participants, who were middle-aged and older, were inquired about their lifestyle and examined in regard to genetic factors. More than 130 lifestyle factors have been analyzed to identify the interaction between environment and genes as obesity facilitators (Flores-Dorantes et al., 2020). The factors include general and psychological health, sleep, physical activity, alcohol use, smoking, nutritional habits, and the GRS. Based on the findings, a broad definition has been postulated concerning gene-environment interaction. The description of the relationship is therefore stated as the response of an individual to environmental stimuli based on their genotype. Thus, the environment confers susceptibility while influencing and modifying the genetic predisposition.
Analysis of United Biobank data yielded results that are significant to the examination of the interaction between genes and the environment. Specifically, physical activity, alcohol consumption, and socioeconomic have been described as the most prominent environmental factors influencing the development of obesity in the presence of genetic risk variants. Moreover, parent feeding behavior and diet have been listed as elements linked to excess weight gain. The environmental circumstances mentioned previously are illustrated as risks correlated with the existing genetic predisposition to obesity.
Individual Aspects of Gene-Environment Interaction in Obesity
Physical Activity
The obesogenic environment connects with physical activity from an energy balance perspective. When it comes to obesogenic conditions, energy balance is examined as its expenditure and intake. In relation to lower energy expenditure, a sedentary lifestyle or physical inactivity interacts with the genetic predisposition, resulting in the development of obesity. Namely, research was conducted in regard to the relationship between exercise and the obesogenic environment. A study analyzing 12 variants that are related to obesity in 20,000 men demonstrated that having an active lifestyle reduces genetic predisposition risks by 40% (Rask-Anderson et al., 2017). A similar meta-analysis study of more than 110,000 individuals supported the previous results, illustrating that physical exercises counterbalance the genetic proneness to developing obesity (Flores-Dorantes et al., 2020). As a result, it can be highlighted that physical activity can be used as a control measure for obesity despite biological inclinations.
Alcohol Consumption
An additional gene-environment factor is alcohol consumption. Rask-Andersen et al. (2017) mention that this is a factor associated with high BMI. In essence, alcohol intake can ameliorate the effects of obesity genetic variants through the lowering of the BMI. This finding is consistent with the data showing that alcoholic patients present lower physical activity yet a lower BMI as a result of a rise in lipolysis and proneness to disorders associated with lipid metabolism (Rask-Anderson et al., 2017). Indeed, it has been demonstrated that chronic alcoholism could ignite lipodystrophy in rats and mice (Flores-Dorantes et al., 2020). Moreover, higher lipolysis and fatty acid secretion initiate the transportation of the fatty acids to the liver, leading to their accumulation and causing hepatic steatosis over time. These analyses have illustrated that an inherently negative environmental factor, namely, alcohol consumption, can positively affect patients with high excess weight.
Economic and Social Status
Various researchers have assessed the relationship between socioeconomic status and the molecular basis of obesity. It has been established that obesity prevalence increases with higher deprivation levels that are attributed to a worse diet and less physical activity. In developed nations, excess weight prevalence is higher among poor people yet affects affluent ones less significantly (see Appendix B). In developing countries, however, obesity is higher in the upper-class individuals of the social hierarchy (Flores-Dorantes et al., 2020). An excellent example is Mexico, a developing nation in which the middle class has the highest potential of becoming obese (Flores-Dorantes et al., 2020). This phenomenon can be explained by assessing the behavioral change of an individual as they move from one social class to another.
Similarly, the effect of a socioeconomic factor, such as education on BMI, can be determined. To address this, the results of an experiment on siblings sharing the same environment are assessed. Researchers highlight that higher academic levels correlate with lower BMI. Therefore, the education aspect affects one’s ability to select, purchase, and consume healthier products (Flores-Dorantes et al., 2020). A similar study performed on children demonstrates that severe obesity increases in rural areas and ones with a low rate of individuals obtaining an education (Ogden et al., 2018). As such, education is associated with BMI through decisions that are informed by knowledge acquisition or information.
Diet
One of the leading environmental elements that impact the genetic factor for obesity is diet. An accelerated lifestyle has altered food intake, influencing people to change their dietary habits. As a result, individuals often opt for less healthy yet more convenient meals instead of being diligent about their nutrient and calorie intake. Specifically, a US Nutritional Survey performed between 1965 and 2008 reported that homemade diets had decreased by 23%, and most Americans consume calories generated through processed goods from restaurants or groceries (Flores-Dorantes et al., 2020). The issue, however, is not a country-based one but a global phenomenon. A study in the United Kingdom demonstrated that the consumption of non-homemade meals correlates with a higher calorie intake (Flores-Dorantes et al., 2020). Comparably, cooking at home is associated with contrasting results as it has been shown to have more nutritional benefits. The alterations in dietary habits portrayed worldwide can be highlighted through the consumption of more calories, which ultimately generates obesity.
Review of Studies on Diet
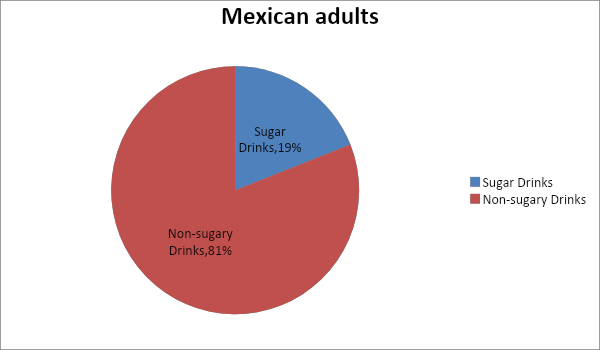
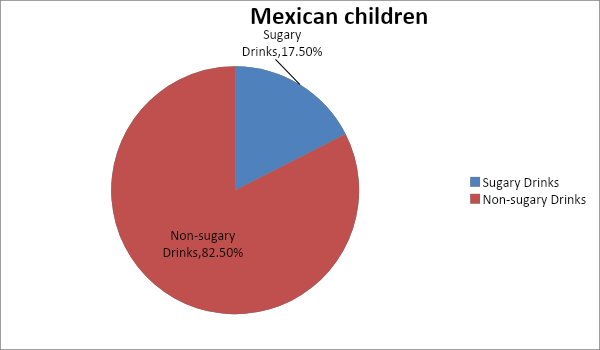
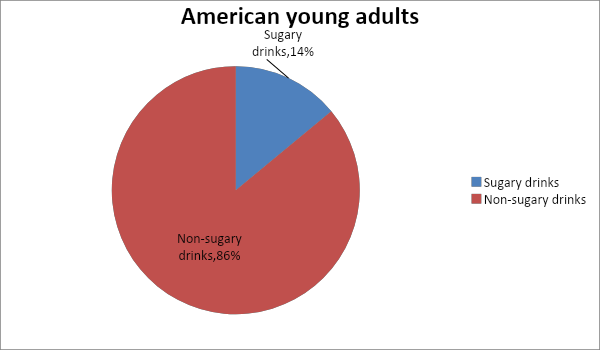
The populations of two countries have been studied by researchers, and the results of the studies have been linked to the interconnection of dietary habits and obesity. The results have shown that, for the period between 2005 and 2010, 14% of American young adults received their calorie needs from sugar-sweetened drinks (Flores-Dorantes et al., 2020). Another notable example is Mexico, which has the world’s highest obesity prevalence. In the country, 19% of adults and 17.5% of children obtained their daily calories from sugary drinks (Flores-Dorantes et al., 2020). Evidently, sugar intake is, to an extent, a circumstance for the molecular basis of obesity.
In addition to the studies conducted on the two countries, specific systematic reviews have also established a relationship between sugary food consumption and the prevalence of obesity. An analysis of 32 studies has demonstrated a positive association between sugar-sweetened beverage consumption and obesity risk. Additionally, a meta-analysis showed that consumption of beverages has risen over the years, and 75% of soft drinks and food contain added sugar. Indeed, drinking sugar-sweetened beverages increases the risk of obesity, metabolic syndrome, and diabetes (Flores-Dorantes et al., 2020). Moreover, obesity-genetic predisposition is associated with a positive correlation between beverage and dried food consumption and adiposity traits (Flores-Dorantes et al., 2020). An additional review suggested that frequent consumption of dried foods generates a higher risk of developing adiposity and other chronic conditions such as type 2 diabetes (T2D) and hypertension (Flores-Dorantes et al., 2020). Results from similar studies illustrate that eating more fruits and vegetables and avoiding red and processed meat ameliorates cardiometabolic profiles. Based on the aforementioned information, constant consumption of sugar additives in foods is linked to high obesity prevalence rates.
The results of the studies on the relationship between obesity and diet have impacted the recommendations regarding nutritional needs across the world. Based on the effect of diet on the development of obesity, the World Health Organization has published dietary guidance that promotes a higher intake of fruits, vegetables, legumes, grains, and nuts. The WHO recommendations limit the consumption of sugar and fat to not more than 10% and 30%, respectively, of the total calorie intake (World Health Organization, 2018). One’s diet is a portrayal of the interaction between humans and the environment. Disadvantageously, the production of meat and fresh produce for consumption is linked to an environmental change through the unsustainability of biodiversity. An additional drawback to the dietary recommendation is the fact that socioeconomic status marginalizes a section of a population in accessing healthy food, therefore making a healthy diet impossible to maintain. Apart from understanding the basis of obesity through the connection between dietary habits and genotypic traits, it is also worthwhile to notice that adhering to specific food intake traits can become a barrier due to one’s experienced environmental and socio-economic barriers.
Another essential factor that is to be considered is the multiple elements the environment consists of. Thus, a sequencing framework can be inefficient due to the numerous variables and factors that may have an impact on obesity. As a result of the phenomenon, sequencing the human genome appears to be a less unattainable goal. Human genome sequencing can facilitate a more thorough understanding of geniting mutations generating or worsening obesity cases. Moreover, the approach correlates with new research on the multiple genetic variations that can maximize genetic susceptibility to excess weight.
Development-Environment Interaction in Obesity and Intervention
The third interaction that contributes to obesity is the linkages between the environment and the biological development of behaviors. People’s inclinations and health are influenced by various elements of the built environment, including geographical allocations, access to nature, color, indoor air quality, noise, thermal comfort, user control of space, and preferences (Nagaraj, 2020). These factors interact with the growth of a person and the development of actions and patterns that lead to obesity. Nevertheless, not all the aforementioned elements can provoke behaviors that can ignite adiposity.
Interactions in Obesity Cause
Numerous studies show the positive effects of daylight on human psychological traits and well-being. In the field of healthcare, for instance, many studies show that valetudinarians placed in well-lit rooms recover more quickly as opposed to those assigned to dark-lit rooms (Nagaraj, 2020). Remarkably, the presence of a psychological relationship between an environmental component such as light and the development of specific characteristics are evident. These characteristics lead to the formation of particular inclinations that are associated with obesity. Additional studies reveal that individuals experiencing obesity are more likely to suffer from anxiety and depressive disorders (Sagar & Gupta, 2018). Such people have been found to have problems with eating behavior and overall quality of life, namely from the perspective of physical activity. Deductively, psychological symptoms have adverse implications on the quality of life, self-esteem, and nutritional habits. Undoubtedly, the poor eating attitudes that are adopted by an individual are a result of one or more environmental elements that shape one’s behavioral patterns and relationship with food and sports.
Access to a green environment has also been proven to have an indirect correlation with obesity. It has been found that interactions with nature yield better cognitive functioning, increased self-discipline, impulse control, and adequate overall psychological health (Nagaraj, 2020). Biologically, the weight of an individual is controlled in the hypothalamus, which is a small area at the base of the brain, situated in the midline behind the ears. However, several studies have revealed that the brain’s prefrontal cortex, which is associated with complex planning and self-control, is smaller in people who tend to overeat (Nagaraj, 2020). As a result, it can be stated that individuals who overeat or have the tendency to consume high-energy level foods may have a poorly developed prefrontal. In regards to external circumstances, limited access to nature is associated with exacerbated attention deficit, higher rates of anxiety disorders, and increased cases of mental illnesses such as depression (Nagaraj, 2020). An explanation is that an individual with an undeveloped prefrontal cortex may have been exposed to less or no green environments, which, in turn, affects cognitive functioning.
The development and establishment of personal traits are also known to determine obesity status throughout the life of an individual. Many reviews have focused on personality traits, mainly in the adult population. Notably, personality traits such as conscientiousness increase along the life course, while obesity-prone behaviors decrease with age (Jiang et al., 2022). In the lower stages of development, such as childhood and adolescence, conscientiousness is lower compared to the same variable in older demographics. Thus, making decisions on issues related to nutrition can be more effective based on the environmental and developmental characteristics of a person. Additionally, a trait that is also impacted by one’s environment is openness, which facilitates a sense of curiosity concerning certain foods that have been linked to excess weight gain (Jiang et al., 2022). In this case, it is not a single environmental factor that interacts with the development of a child but a variety of elements. Media, friends, social groups, and parents may either generate or combat nutritional habits correlating with obesity.
Interactions in Obesity Intervention
Environmental factors interact with other human development elements in obesity interventions. A suitable example is the social connections and influence of one’s friends. If an obese individual is surrounded by a group of acquaintances who are not obese, two scenarios can unfold. On the one hand, the friends may develop excess weight because of the adoption of new eating habits from the individual with different dietary habits. Secondly, the obese individual may copy the conduct that can help in reducing excess weight. Since obesity in itself is a disorder, there is a greater likelihood that the second scenario will take place. Thereby, the person with weight problems will see a systematic behavioral improvement. The adoption of behaviors that discourage binge eating is one of the interventions that are important in reducing obesity prevalence or controlling adiposity levels. The phenomenon and nutritional patterns alter based on outside interactions, and, as a result, the person with weight issues is more likely to have a more moderate approach to sugar and fast food. Furthermore, such changes can be generated through information sharing and encouragement.
On the other hand, food availability is an environmental factor linked to the employment of obesity intervention. The food vendor in one’s neighborhood can determine the types of food the resident’s purchase (Lee et al., 2019). For example, a person located in a food desert where the only nutritional sources are gas stations cannot easily access fresh produce unless the individual has a vehicle. On the other hand, certain areas may mainly have fast food restaurants, which creates circumstances in which individuals cannot remain motivated to adhere to healthier eating habits. However, the argument can be applied to an instance in which an individual is in close proximity to markets and health food stores, ultimately leading to the formation of better nutritional patterns. A review of certain studies has found that the opening of supermarkets in the area has a positive impact on the quality of the food consumed by the local demographic yet has no positive correlations with changes in BMI and higher consumption of fruits and vegetables (Lee et al., 2019). Based on the aforementioned information, it can be stated that stores mainly offering healthy foods can have a positive effect on the health of the population living nearby. Thus, an obesity intervention starts with the establishment of an environment in which healthy food is available and accessible.
There is an intricate way in which an external factor, such as transportation and infrastructure, impacts obesity rates. An area’s infrastructure can dictate whether people can walk to specific locations without driving, which would have a positive effect on one’s physical activity and, hence, weight control. High neighborhood walkability is associated with decreased prevalence of overweight and obese residents (Lee et al., 2019). An element that is to be considered is walking as an intervention that is both accessible and relatively easy to implement. Thus, obesity intervention aiming to operate on a large scale starts with the environment in which individuals operate.
Conclusion
It is certain that interactions between environmental factors, development, and genetics have an implication for the molecular basis of obesity. Genetic factors are found to have a more significant effect on the basis of obesity in childhood compared to the same element affecting the childhood stage. The phenomenon can be formulated as the prevalence of genetic effects in childhood altered through the preponderance of environmental ones for adults. In regard to genes and development, obesity can be monogenic or polygenetic. Changes such as genetic mutations are known to cause monogenic obesity. On the other hand, polygenetic obesity is characterized by the polymorphism of several genetic variants. Genes that are associated with obesity have also been linked to the development of the CNS and neurogenesis. Essentially, development is linked to one’s genetics concerning the potential chronic risks correlating with weight gain, especially in children.
Current reviews of medicinal reports have indicated that there is a high likelihood of developing obesity based on the interactions between genes and the environment. A significant observation recorded by scientists is that genetic factors are the primary causative agents in the molecular basis of excess weight gain. Researchers employ frameworks such as the GRS to determine said relationships and establish the leading causes impacting an individual’s condition. Additional research that has been crucial to the formulation of interventions is the analysis of the obesogenic environment and its impacts on the organisms that continually interact with it. Various reviews have been conducted to determine the environment and factors facilitating obesity. The results generated from such studies have revealed a high likelihood of certain external elements minimizing or maximizing the cases of excess weight gain. The samples collected by organizations such as United Biobank have been examined to establish the gene-environment interaction. Information from the studies has formed the foundations under which nutritional health guidelines are drawn.
The third interaction crucial in understanding the molecular basis of obesity and intervention is the development-environment one. There has been limited research on this interaction. However, the impacts of the connections are manifested in the processes in which said patterns can cause obesity. The results are evidenced in the health and nutritional behavior of humans. Therefore, impacts that can be attributed to the environment-development link are the indirect effects on human behavior. Specifically, the behaviors developed in the progression of obesity and interventions are the outcomes of the intertwined correlation between environment and one’s physical and psychological growth. Future research studies are to focus on the interaction between human behavior and genetic factors in obesity and intervention. The strength of this review is the framework applied to elucidate the indirect impacts of various biological, social, cultural, and physiological elements on obesity rates.
References
Flores-Dorantes, M., Diaz-Lopez, Y., & Gutiérrez-Aguilar, R. (2020). Environment and gene association with obesity and their impact on neurodegenerative and neurodevelopmental diseases. Frontiers in Neuroscience Journal. Web.
Jiang, D., Huang, T., Chen, J., Xiao, W., & Liu, Z. (2022). The association of personality traits with childhood obesity: A systematic review and meta-analysis. MedRxiv. Web.
Khera, A., Chaffin, M., Wade, K., Zahid, S., Brancale, J., & Xia, R. (2019). Polygenic prediction of weight and obesity trajectories from birth to adulthood. Cell (177), 587–596. Web.
Lee, A., Cardel, M., & Donahoo, W. (2019). Social and environmental factors influencing obesity. In K. Feingold et al. (Eds.) Endotext: Comprehensive free online endocrinology book. Web.
Nagaraj, G. (2020). Impact of environment on human behavior. The Times of India. Web.
Ogden, C., Fryar, C., Hales, C., Carroll, M., Aoki, Y., & Freedman, D. (2018). Differences in obesity prevalence by demographics and urbanization in US children and adolescents, 2013-2016. JAMA 319, 2410–18. Web.
Rask-Andersen, M., Karlsson, T., Ek, W., & Johansson, Å. (2017). Gene-environment interaction study for BMI reveals interactions between genetic factors and physical activity, alcohol consumption, and socioeconomic status. PLoS Genet. 13, e1006977. Web.
Sagar, R., & Gupta, T. (2018). Psychological aspects of obesity in children and adolescents. The Indian Journal of Pediatrics, 85(7), 554-559. Web.
World Health Organization. (2018). Healthy diet. World Health Organization. Web.
Appendix A
Appendix B