Introduction
The publication of To Err Is Human was a watershed moment for healthcare history, as it brought the problem of patient safety to the public. This milestone encouraged the development of numerous standards and interventions that helped improve patient safety. Wachter (2010) wrote that five years after the milestone publication, the improvements were tremendous. Agencies developed appropriate regulations, created incentives for health information technology growth, emphasized malpractice systems, and promoted workplace training. Today, twenty years after the milestone, government agencies developed numerous quality measures that help to keep track of quality improvements in healthcare organizations and create hospital ratings so that patients can compare the quality of services. The present paper describes three of such quality measures by deconstructing them, emphasizing their importance, and discussing their impact on healthcare costs.
Communication with Nurses
Deconstructing the Measure
Communication with nurses is one of the quality measures for hospitals evaluated by the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey, which is an annual study conducted by Centers for Medicare and Medicaid Services (CMS). Communication with nurses is measured by the first three questions that allow patients to evaluate how well hospital nurses treated them. Communication with nurses is defined as the quality of patient-nurse communication as perceived by patients. The quality measure shows if nurses treated the patients with courtesy and respect, listened attentively, and explained everything well (CMS, 2021a).
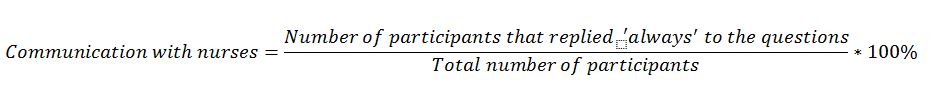
The measure is calculated as a percentage of people that replied to the first question in HCAHPS “always.” In other words, communication with nurses is measured using the following formula:
The data is collected on an annual basis through a nationwide survey. The patients are carefully selected according to an intricate sampling method to reduce bias (CMS, 2021). The survey is conducted by phone or by email in English and Spanish, depending on the patient’s preferences.
The measure is compared externally to the state and national averages. If the hospital’s rating in terms of nurse communication is below the average percentage, it demonstrates that patients’ experience of communicating with nurses was not as good as patients would expect. The percentile ranking is not provided for this measure. However, it is also a part of the five-star patient survey rating, which allows comparison among different hospitals.
The measure is risk-adjusted, as it takes into consideration the population a hospital serves. Adjusting for risks makes allows better among hospitals. CMS analyzes the sample characteristics to understand if the sample collected for one hospital differs in social factors, such as socioeconomic status or ethnic background (CMS, 2021). After that, a statistical model for calculating the measure is moderated according to the characteristics of the sample.
If an organization aims at excelling in the market performance, it should consider aiming at having the measure at a level significantly above the average. For instance, in 2020, 80% of patients reported that nurses communicated well to them on average in the US (Medicare, 2021). So an organization that aims at an advanced market performance should aim at the rate of 85% and above.
Importance
Nurse communication is an essential measure that affects all spheres of care provision. Nursing is a science that studies how to care for humans as bio-psycho-sociological beings (Kourkouta & Papathanasiou, 2014). This implies that nurses are to know how to care for their patients’ biological, psychological, and sociological needs. Adequate communication is a sociological as well as a psychological aspect of nursing care. If nurses understand the psychological needs of a patient, they need to use their best social skills to satisfy these needs. Thus, nurse communication is a critical factor that measures the professionalism of nurses. By seeing nurse communication ratings, patients can evaluate the quality of nursing care in an organization and select the one they like the most (CMS, 2021a). Therefore, healthcare organizations are motivated to ensure that their nurses communicate with patients at the top level. As a result, they may consider providing on-the-job training or offer rewards for top-class patient communication.
Nurse communication skills are crucial for all the areas of the nursing process. In particular, nurse communication facilitates prevention, treatment, therapy, rehabilitation, education, and health promotion (Kourkouta & Papathanasiou, 2014). Nurse communication is a two-way process. On the one hand, the patient tells the nurse about all the concerns and problems to resolve them. On the other hand, the nurse transfers the knowledge to the patients about their conditions and treatment options to ensure the fastest recovery. Effective communication with nurses helps the nurse to assess the patients’ condition, understand their needs, and explain how these needs can be satisfied (Kourkouta & Papathanasiou, 2014). Therefore, top-level nurse communication is vital for the provision of high-quality care.
Patient Safety and Cost of Care
Nurse communication has a significant impact on patient safety. Burgener (2020) claims that ineffective nurse communication has been a matter of numerous adverse events and unfavorable patient outcomes. Thus, it is crucial to improve nurse communication through systematic training and creating incentives for improvement (Burgener, 2020). Effective nurse communication allows receiving valuable information about the patient at the right time, which is crucial for adequate and timely care (Kourkouta & Papathanasiou, 2014). Without such communication, it is impossible to establish a functional patient-nurse relationship. Additionally, nurse communication allows effective teamwork, smooth transition of patients, and collaborative care, which are crucial for patient safety (Burgener, 2020).
There are no studies that discuss the direct relationship between the cost of care and nurse communication. However, it is clear that there is an indirect link between the cost of care and nurse communication. World Health Organization (WHO, 2017) stated that ineffective patient safety practices cost trillions of dollars to healthcare systems worldwide due to adverse outcomes. Moreover, the psychological cost of adverse outcomes to patients, their friends, and family are priceless (WHO, 2017). Therefore, it may be concluded that patient safety acts as a mediator of the relationship between nurse communication and cost of care. The relationship between these two concepts is negative, which implies that the better nurse communication, the lower the cost of care.
Rate of Readmissions for Heart Failure Patients
Deconstructing the Measure
Rate of readmission for heart failure patients is a measure included in the evaluation of unplanned hospital visits. The measure is defined as the number of patients that returned to the hospital within 30 days after their additional discharge (CMS, n.d.a). The condition that served as a reason for readmission is not relevant, as all patients that returned to any hospital within 30 days are added to the readmission rate (CMS, n.d.a). The quality measure aims at determining how well a hospital implements preventive practices to ensure that patients do not have complications.
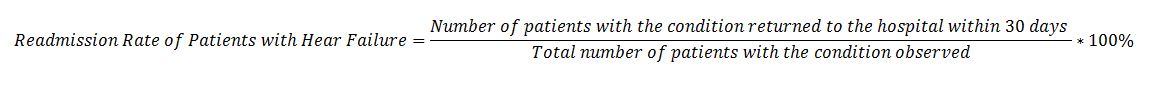
The readmission rate is calculated by dividing the number of people that returned to the hospital within 30 days by the total number of people observed with the condition and multiplying by 100%. In other words, the total number of patients observed or treated in a hospital with heart failure goes in the denominator, and the number of people among these patients that returned to the hospital within 30 days goes to the numerator. The formula for the measure can be written down as follows:
The data is collected using Medicare claims data and eligibility data. In other words, CMS collects data retrospectively by analyzing Medicare claims of people hospitalized with heart failure and checking how soon they were readmitted to a hospital after their initial visit. The readmission rate is calculated for Medicare beneficiaries aged 65 or older “enrolled in Original Medicare for at least 12 months before their hospital admission and maintained enrollment through 30 days after their original discharge” (CMS, n.d.a, para. 6). CMS (n.d.a) reports that using Medicare claims is a more accurate data collection method in comparison with hospital charts when estimating the readmission rates.
The quality measure is compared externally by including a hospital into one out of three groups (CMS, n.d.a). The groups are those hospitals that performed better than average, the same as average, and worse than average. If a hospital’s 95% confidence interval is below the national average, the hospital is known to perform “better than the national rate.” If a hospital’s 95% confidence interval includes the national average, the hospital is known to perform “no different than the national average. Finally, if a hospital’s 95% confidence interval is entirely above the national average, the hospital is known to be “worse than the national rate” on the measure. Hospitals that have fewer than 30 cases of the condition during the reporting period are not evaluated by the measure. Hospitals may also be compared to each other by evaluating the quality intervals of their readmission rates.
The measure is risk-adjusted, as it considers a number of factors that may contribute to the risk of being readmitted to the hospital. In particular, CMS (n.d.a) reports that it adjusts the risks according to a patient’s age, past medical history, and co-morbidities. This allows more reliable comparison of different hospitals.
A healthcare organization that wants to excel in the quality of provided services should aim at being included in the group “better than the national rate.” In other words, the confidence interval of the readmission rate should be below 21.9%, which is the current national average (Medicare, 2021).
Importance
The importance of measuring readmission rates is difficult to overstate, as they demonstrate how well an organization performs preventive measures to ensure the best patient outcomes. Unplanned hospital visits disrupt people’s lives and increase the possible adverse events, such as hospital-acquired infections (CMS, n.d.a). Measuring readmission rates is crucial for both hospitals and patients. For patients, readmission rates demonstrate how likely they are to return to the hospital within 30 days after discharge in comparison with the national average. Readmission rate may be a criterion for a patient to select among several healthcare organizations. Measuring readmission rates also incentivizes hospitals to improve their internal practices to reduce readmission rates. Improvements that allow reducing readmission rates are often very costly, and hospitals are not likely to make significant capital investments without adequate incentives (Steventon & Billings, 2017). Measuring readmission rates crates such incentives for hospitals.
Patient Safety and Cost of Care
Readmissions have a negative impact on both patient safety and the cost of care. As it has been mentioned earlier, readmissions are associated with increased risks of hospital-acquired infections (CMS, n.d.a). At the same time, preventable readmission increased the cost of care, as they show that the costs associated with readmissions could have been avoided (Phillips et al., 2019). Hospitals are now financially responsible for readmissions, which implies that it is of increased interest to reduce readmission rates associated with all conditions, including heart failure.
Death Rate for Pneumonia Patients
Deconstructing the Measure
The death rate for pneumonia patients is a critical quality measure during the pandemic due to the increased number of pneumonia cases worldwide. The measure is defined as the number of patients reported dead thirty days after admission to the hospital (CMS, n.d.b). The rate is measured within 30 days because deaths after this period may be associated with another condition. The rate is calculated similarly to the two previous rates discussed in the present paper. The formula for death rate for pneumonia patients is provided below:
Death rates are measured using Medicare claims and eligibility data. This allows fast data collection without having to review medical charts (CMS, n.d.b). Similar to readmission rates, mortality from pneumonia is also measured for patients aged 65 or older eligible for Medicare at least a year before admission to the hospital with pneumonia (CMS, n.d.b).
The measure is compared externally on the same principle as the readmission rates. Hospitals are also classified into three groups based on this quality measure: those that before above, below, or at the same level as the national average. The quality measure is risk-adjusted, taking into consideration the patients’ age, medical history, and co-morbidities.
An organization that aims at excelling in the quality of care should aim at performing above the national average. Currently, the average death rate among pneumonia patients is 15.3% (Medicare, 2021). Therefore, such organizations should aim at having mortality rates from pneumonia at 12.5% or below. The organizations should remember that significance testing is applied to the rating, which implies that small differences between the average national mortality rate for pneumonia and the hospital’s pneumonia mortality rate will not put the hospital in the group of hospitals that perform above the national benchmark.
Importance
The importance of the measure is evident, as it concerns preventable mortality. Patient deaths have a negative impact on the psychological health of friends and family. Additionally, having large mortality rates may create a negative reputation for a hospital. Measuring preventable deaths creates incentives for the hospital to implement preventive measures for reducing mortality from pneumonia. As a result, more people have favorable outcomes after being treated for pneumonia.
Patient Safety and Cost of Care
Measuring mortality from pneumonia has a positive impact on patient safety. The quality measure incentivizes hospitals to implement preventive care for pneumonia patients to reduce mortality (CMS, n.d.b). As a result, more patients have positive pneumonia outcomes (CMS, n.d.b). Implementing preventive care has significant capital costs; however, these costs are paid back in the long run due to decreased numbers of readmissions, lawsuits, and complications (Kramer et al., 2017). Thus, measuring death rates for pneumonia patients is critical for both patient safety and the cost of care.
Conclusion
The present paper focused on three quality measures applied to hospitals in the US, including communication with nurses, rate of readmission for heart failure patients, and rate of death for pneumonia patients. The analysis revealed that all the quality measures have either direct or indirect impacts on patient safety and the cost of care. In particular, these measures provide patients with an opportunity to select the best hospital according to the measures of their interest. Additionally, the quality measures create incentives for hospitals to improve their performance. Thus, the analysis revealed that using quality measures is of extreme importance to improve patient experience and outcomes.
References
Burgener, A. M. (2020). Enhancing communication to improve patient safety and to increase patient satisfaction. The health care manager, 39(3), 128-132.
Centers for Medicare and Medicaid Services. (2021a). CAHPS® Hospital Survey (HCAHPS): Quality assurance guidelines. CMS. Web.
Centers for Medicare and Medicaid Services. (2021b). Risk Adjustment in Quality Measurement. CMS. Web.
Centers for Medicare and Medicaid Services. (n.d.a). Unplanned hospital visits. Web.
Centers for Medicare and Medicaid Services. (n.d.b). Complications & deaths. Web.
Kramer, A. A., Dasta, J. F., & Kane-Gill, S. L. (2017). The impact of mortality on total costs within the ICU. Critical care medicine, 45(9), 1457-1463.
Kourkouta, L., & Papathanasiou, I. V. (2014). Communication in nursing practice. Material socio-medica, 26(1), 65-67.
Medicare. (2021). Redmond Regional Medical Center. Medicare.gov. Web.
Phillips, J. L., Rondon, A. J., Vannello, C., Fillingham, Y. A., Austin, M. S., & Courtney, P. M. (2019). How much does a readmission cost the bundle following primary hip and knee arthroplasty? The Journal of arthroplasty, 34(5), 819-823.
Steventon, A., & Billings, J. (2017). Preventing hospital readmissions: the importance of considering ‘impactibility,’not just predicted risk. BMJ quality & safety, 26(10), 782-785.
Wachter, R. M. (2010). Patient safety at ten: unmistakable progress, troubling gaps. Health Affairs, 29(1), 165-173. Web.
World Health Organization. (2017). Patient safety: making health care safer. World Health Organization. Web.
