Introduction
India is the second most populous country in the world today after China. This South Asian nation has promoted notions of democracy in an effort to promote governance and support more citizens to record positive health outcomes. The reason behind selecting this nation for this study is because it has a good healthcare system despite having a population of over 1.4 billion citizens (Malik, 2022). Having been in the country for a while, I have realized that most of the individuals are usually able to access or afford medical services. From a professional perspective, India stands out as a country with improved processes and technologies that explain why medical tourism has become a common feature. The approach would shed more light regarding this nation’s healthcare sector and how it was prepared to meet future demands of its population. The analysis would also expose some of the strengths that made the industry successful and the major opportunities for consideration. The study would go further to pinpoint key challenges that administrators of healthcare and citizens face within the country’s healthcare system.
To complete the investigation, I identified a number of resources that were capable of providing high-quality and meaningful information about the country’s health sector. First, most of the government agencies and ministries in the country own and operate websites that are useful in disseminating data and emerging insights about the sector. Such sources were capable of providing the much needed ideas. Second, I was able to identify a number of journal articles published within the past three years. Such resources were peer-reviewed and capable of providing verified information. Third, I identified several books focusing on the Indian healthcare sector. Fourth, the consideration of some of the leading hospitals and their websites made it easier for me to complete the investigation successfully. This presentation means that the sources were timely and capable of delivering the much needed information. Throughout the study period, I observed that there were no difficult terms or phrases. Consequently, I managed to complete the investigation successfully and within the stipulated timeframe.
Description of India’s Public Health System
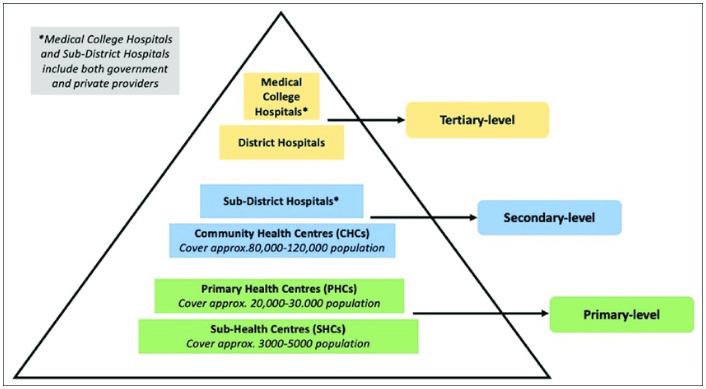
The healthcare system of India is designed in such a way that can meet the health needs of more citizens. To deliver the intended goals, the government has established primary, secondary, tertiary, and specialized medical facilities that are found across the country. On top of these levels, there are other primary institutions intended to provide medical services to the people. Tertiary centers are at the apex of the care sector and help meet the demands of patients who have been referred from secondary and primary healthcare institutions (Sheeba and Anbu, 2020). Some of them include medical college and district hospitals (see Fig. 1). Secondary level institutions include sub-district hospitals and community health centers (see Fig. 1). The primary level is characterized by sub-health centers (SHCs) and primary health centers (PHCs). All the existing healthcare institutions in the sector share information and engage in coordinated efforts to meet the needs of the country’s population.
Main Players and Institutions
Issues to do with health policy in India are handled and managed by the Ministry of Health and Family Welfare. Under the leadership of the government, the ministry is tasked with formulating approaches and strategies that could be implemented across the country. This ministry liaises with other departments and agencies to focus on the issues to do with medical services (Sheeba and Anbu, 2020). These departments share emerging details and liaise with other key administrators in the subsequent levels. The tertiary institutions have leaders who liaise with the ministry and the relevant departments to support public health administration (Tikkanen et al., 2020). The ministry goes further to monitor and makes timely decisions regarding the issue of family planning. The ultimate role is to ensure that most of the citizens are able to achieve proper medical support while keeping the population under control.
Across the nation, the Ministry of Health and Family Welfare Ministry plays a critical role of coordinating operations to ensure that secondary and primary institutions are aware of their functions and specific undertakings to meet the population’s health needs. Based on this analysis, it is evident that the country does not promote overlap of functions (Sheeba and Anbu, 2020). The government engages in policy planning and feasibility studies that are considered when formulating new guidelines. These efforts have continued to help the relevant leaders in the healthcare to meet the changing demands of more people across the country.
Major Problems for Public Health Administrators
Just like in most of the Asian countries, public health administrators in India continue to encounter a number of challenges that disorient the quality of services available to most of the patients. For instance, the professionals acknowledge that most of the present caregivers and health experts are understaffed. This happens to be the case since the country is one of the most populous in the world. The health sector of India also lacks proper strategies for identifying volunteers who can continue to offer care to patients in the country (Tikkanen et al., 2020). These human resources (HR) issues have the potential to disorient the overall efficiency of the public health sector. This problem is associated with increasing cases of burnout and turnover among the workers in different levels of care delivery. In the recent past, the country’s efforts to increase the overall level of workforce have not delivered meaningful results.
Scholars have identified India as one of the countries with advanced technologies in healthcare. However, the continued adoption of modern technologies to merge primary, tertiary, and secondary medical facilities has led to additional challenges. Some of them include poor referral outcomes whereby there is a system breakdown and lack the necessary skill sets among medical workers. In rural settings, gaps in skill sets exist, thereby making it impossible for the country to record most of the targeted health outcomes (Hooda, 2021). Additionally, administrators in the sector find it hard to address these problems. Another issue is that the overall health care system has a number of inefficiencies in the handling of community-based services.
As described above, it is notable that India is one of the countries whose public health sector characterized by different levels. Based on this understanding, it is agreeable that most of the administrators find it hard to restructure the best approaches to promote systematic assessments (Hooda, 2020). Such gaps explain why primary centers at the bottom of the framework find it hard to offer personalized services. The recorded population in India makes it hard for the established system to continue delivering the much needed services (Hooda, 2021). The government has also failed to consider a number of improvements that could transform the experiences of more citizens, such as increased levels of insurance cover. These challenges different administrators face in the country explain why proper changes would be needed in the future. The considerations of evidence-based and timely approaches could set the stage for better and personalized services. More administrators would also find it easier to streamline most of their operations and transform the overall image of India’s health sector.
India’s Health Policy
The health sector of India pursues its goals through the National Health Policy (NHP). This initiative is tasked with several responsibilities, such as informing and promoting the major governmental roles to ensure that they focus on people’s health outcomes. The 2020 NHP focuses on increased expenditures on health from 1.15 to 2.5 percent of the national GDP by the year 2025 (India Filings, 2022). The government liaises with the Council of Health and Family Welfare and other key committees to formulate policies and plan for the future of the country’s health outcomes. These efforts are pursued in line with the challenges affecting the sector. For instance, the country’s population forms the primary source of concern. According to Hooda (2021), India has a population of around 1.4 billion. The rate has been increasing at a rate of around 0.9-1 percent annually. This scenario means that the government should have proper mechanisms to ensure that all citizens are able to get timely services.
Several health challenges exist in this country that might affect the overall outcomes or success of the sector. For instance, cancer has become one of the terminal conditions affecting around 10 percent of the population (Tikkanen et al., 2020). This issue increases the overall burden on the economy. Other conditions more people continue to encounter in this country include obesity, heart diseases, and diabetes (India Filings, 2022). In another analysis, Hooda (2021) observed that rural India was grappling with other diseases, including tuberculosis, pneumonia, diarrhea, worm infestations, and malaria. Most of these illnesses were directly associated with increasing morbidity in such areas. Public funding for health services remained low in comparison with individuals who were receiving medical services from the private sector.
Some analyses completed in the recent past have presented a number of issues facing the Indian population. For instance, a peculiar trend is notable whereby infrastructural gaps in healthcare continue to exist. Specifically, the annual growth rate of the Indian economy is not directly connected to overall improvement in the sector. Some of the challenges the government needs to start taking seriously is that of both non-communicable and communicable illnesses (Tikkanen et al., 2020). The country also lacks adequate bed capacity that could meet the overall demand of the wider population. This problematic issue is supported by the fact that only 1.5 beds are only available to every 1000 people (Indus Health Plus, 2022). The consideration of these issues could help the relevant authorities to formulate a superior policy that could help the country to record positive outcomes in the coming years.
Current Health Interventions and Reflection on the Health Policy
The question of health remains complex due to India’s physical size and population. The government has instituted several agencies that collaborate with existing facilities to support the people’s health outcomes. Before the launch of a new five-year plan policy, the National Population Policy (NPP) is involved too assess the rate of population growth and consider the emerging social, political, medical, and economic development needs. Due to nature of these factors, the government promotes the Health Policy Project (HPP) to improve reproductive health and family planning (Health Policy Project, 2022). The aims of the HPP are coordinated with those of the National Institute of Health and Family Welfare (NIHFW) to deliver sustainable results (World Health Organization, 2017). The emerging efforts deliver new policies that can promote the best practices and initiatives to boost cooperation in care delivery.
The latest NHP put in place continues to help and guide all agencies to clarify and prioritize key areas that can deliver the much needed health outcomes. The current policy is focusing on the best approaches to identify emerging medical conditions and implement proper mechanisms to prevent them (Health Policy Project, 2022). A multiagency approach is in place whereby agencies develop the best human resources, include key health facilities, and integrate emerging technologies (Health Policy Project, 2022). The policy ensures that gained recorded in the past continue to guide future efforts and initiatives. Priorities tend to change depending on the experienced challenges in the wider public health sector. For instance, renewed efforts are evident in an effort to deal with maternal and pediatric health challenges.
Within the identified policy framework in place, the government has been relying on evidence-based approaches to ensure that positive results are recorded. For instance, financing is proposed in line with the performance of the economy and the GDP. The increase in funding is essential since it has the potential to reduce the challenges more people in need of high-quality services tend to face. The Indian Public Health Standard (IPHS) is involved in this policy to prioritize specific districts whereby more professionals are needed (Health Policy Project, 2022). The Indian government is also keen to expand the number of health volunteers and community workers. The issue of health management information (HMI) is also included within the wider health policy. The primary focus has been to improve surveillance and establish a superior architecture for maximize data sharing. These policy issues dictate the interventions different agencies tend to put in place in an effort to improve the overall health experiences of the country’s ever-growing population.
Despite the effectiveness of these policies, a number of public health challenges continue to exist, thereby disorienting the medical experiences of more people in this country. For example, more citizens with private care coverage are able to receive high-quality services. However, average Indians would have trouble getting similar support from the sector. The relevant government agencies have analyzed this issue to present the National Health Protection Scheme, also known as Ayushman Bharat (Purohit, 2020). Taxes have been formulated in such a way that they are able to fund this program. It is also notable that around 24 percent of the country’s population lacks health insurance (Purohit, 2020). Additionally, around 7 percent of the population lives below the poverty line due to the expenses incurred from the increasing medical expenses (Purohit, 2020). Those who do not have insurance cover in India encounter difficulties when seeking medical support.
The rural setting remains sidelined whereby majority of the citizens in such regions take longer to get personalized medical services. Communicable diseases remain a major challenge in some of the areas. Mortality rates have been complicated by an increasing number of new infections for malaria, different cancer types, and typhoid. Other common diseases include tuberculosis, measles, and diabetes (Sheeba and Anbu, 2020). The absence of properly coordinated medical systems and healthcare infrastructure presents additional predicaments for most of the citizens. The nature of these issues explains why there is a need for all stakeholders in this country to collaborate and consider evidence-based solutions.
Based on the presented information, it is agreeable that the policies the Indian government has put in place are sustainable and capable of delivering desirable results in the long run. However, some inadequacies exist that should inform future mechanisms and changes in healthcare policy. For instance, their scope appears to be inadequate since they fail to consider the medical demands of people living in rural areas. The coronavirus disease of 2019 (COVID-19) has helped expose some of the gaps and inefficiencies of the public health sector (Malik, 2022). The government has also ignored the possibility of increase insurance cover for health among members of the population. While the policies could deliver the needed outcomes, failure to consider at risk groups and those living below the poverty line remains a challenging issue.
These gaps, therefore, explain why the relevant government agencies should tackle the challenges of poverty and inequality since they are connected directly to people’s health outcomes (Sheeba and Anbu, 2020). The relevant agencies would go further to introduce additional programs and frameworks for ensuring that most of the citizens have access to health insurance. The inclusion of emerging technologies and considering of evidence-based clinical guidelines could also help transform India’s health sector. A renewed focus on each of the identified disease affecting the population would also help improve the overall medical outcomes of the greatest number of citizens.
Recommendations and Conclusion
The completed analysis has identified India as one of Asian countries with effective public healthcare systems. The involvement of different agencies and committees allows the government to link all other elements of the economy with the anticipated health outcomes. The relevant departments involved in national planning examine the recorded GDP and suggest the most appropriate financial resources that can meet the outlined NHP policy objectives. Despite the nature of these strategies, a number of challenges affect the effectiveness of the wider healthcare sector (Kasthuri, 2018). Some of the identified ones include chronic and communicable diseases, lack of insurance cover for some, and neglect of rural communities.
Progressive policies focusing on the underserved members of the community could help improve the current situation. For example, there is a need for the government to ensure that additional funds are available to increase the number of people who have access to health insurance (Hooda, 2017). Efforts to hire more professionals and an expansion of facilities and beds would help improve the overall access to medical services. The country can go further to integrate emerging technologies and ensure that they can help improve care delivery (Hooda, 2021). The introduction of emerging clinical guidelines from other countries could help transform the overall efficiency of India’s healthcare sector.
In conclusion, India’s increasing population forms the basis for pursuing proper policies that can help improve medical care delivery to the targeted citizens. The suggested recommendations are capable of helping the government transform the country’s healthcare system within the next few years. Such changes need to be founded on the established policies, levels, and departments to ensure that they deliver sustainable results in a timely manner. The relevant authorities can identify evidence-based approaches to maximize insurance cover, improve access to preventative medical support, and reduce disparities in healthcare delivery.
References List
Health Policy Project (2022) India. Web.
Hooda, S.K. (2017) ‘Health payments and household well-being: how effective are health policy interventions?’, Economic & Political Weekly, 52(16), pp. 54-65. Web.
Hooda, S.K. (2020) ‘Health system in transition in India: journey from state provisioning to privatization’, World Review of Political Economy, 11(4), pp. 506-532.
Hooda, S.K. (2021) Health sector, state and decentralised institutions in India. New York: Taylor & Francis.
India Filings (2022) National Health Policy. Web.
Indus Health Plus (2022) Public health in India: issues & challenges. Web.
Kasthuri, A. (2018) ‘Challenges to healthcare in India – the five A’s’, Indian Journal of Community Medicine : Official Publication of Indian Association of Preventive & Social Medicine, 43(3), pp. 141-143.
Malik, M.A. (2022) ‘Fragility and challenges of health systems in pandemic: lessons from India’s second wave of coronavirus disease 2019 (COVID-19)’, Global Health Journal, 6(1), pp. 44-49.
Purohit, B.C. (2020) Economics of public and private healthcare and health insurance in India. New Delhi: Sage.
Sheeba, A. and Anbu, S. (2020) International issues on health economics and management. New Delhi: TISSL International Publications.
Tikkanen, R. et al. (2020) International health care system profiles: India. New York: Common Wealth Fund.
World Health Organization (2017) Kuwait: country cooperation strategy at a glance. Geneva: WHO.
