The artificial pancreas is also known as a closed-loop system for automated insulin delivery (Boughton & Hovorka, 2019). It is essentially a closed-loop glucose-responsive insulin delivery system guided by a real-time sensor to attend to insulin needs of any variability (Boughton & Hovorka, 2019). The device consists of three essential parts that are connected together to inject insulin whenever it is needed (Kesavadev et al., 2020). The first part is a sensor that measures blood glucose levels and information to a computer (Kesavadev et al., 2020). The second part is the algorithm center that analyzes all the inputs and sends a signal to the insulin pump concerning the required dose of insulin (Kesavadev et al., 2020). The third part is an insulin pump that sends insulin directly to the blood stream to sustain the optimal level of glucose in the blood (Kesavadev et al., 2020). While the name “artificial pancreas” sounds like an invasive device implanted into a patient’s body, it is a wearable device that can easily be replaced without morbidity and mortality. The device is used in medicine to control hyperglycemia in patients with Type 1 diabetes. Thus, the main beneficiaries of the device are patients with Type 1 diabetes. However, US Food and Drug Administration approved the use of the device for patients only above 16 years old (Kesavadev et al., 2020). Therefore, patients with Type 1 diabetes under 16 are not beneficiaries of the device. Figure 1 below visualizes the device.
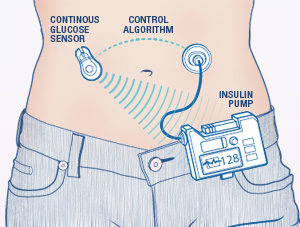
The sensor of the device is attached to the body of a patient so that it can have direct access to the bloodstream. The artificial pancreas measures the level of glucose in the blood in real time and sends the measurements to the algorithm center using a wireless connection (Kesavadev et al., 2020). The algorithm center processes the information to understand when and how much insulin is needed to sustain an optimal level of glucose in the blood (Kesavadev et al., 2020). The data processing center sends the information to the insulin pump that releases a very precise amount of insulin, which is recognized by the glucose sensor. This is why the artificial pancreas is known as a closed-loop system. Figure 2 below visualizes the process of insulin delivery schematically.
The device is based on the concept of glucose control and hormones. Glucose control is of extreme importance for the human body, as it helps to help to prevent numerous conditions. In particular, controlling blood sugar can prevent the development of heart-related conditions, such as infarction, amputation, and stroke (Reaven et al., 2019). Additionally, blood glucose level affects a person’s mood and the level of energy (Grigolon et al., 2019). The human body controls the level of blood sugar using two hormones, including insulin and glucagon. When a person eats, the glucose level in the blood rises, which gives a single to the pancreas to develop insulin, which lowers the level of blood sugar by helping to absorb glucose (Szablewski, 2020). Glucagon works as an antipode of insulin. It gives the signal to release sugar to the blood, when it is too low (Szablewski, 2020). Thus, the pancreas controls blood sugar in a healthy body using two hormones.
Type 1 diabetes is a condition when the pancreas does not develop a sufficient amount of insulin to control blood glucose. Thus, an artificial pancreas is designed to help the human body process glucose. There are two basic types of devices, insulin-only systems and dual-hormone systems (Peters & Haidar, 2018). Insulin-only artificial pancreas monitors the level of sugar in the blood and injects insulin when necessary (Kesavadev et al., 2020). Dual-hormone artificial pancreas also helps to increase blood sugar, which protects patients from hypoglycemia, which is a low level of blood sugar (Peters & Haidar, 2018).
There are two central benefits of an artificial pancreas for patients with Type 1 diabetes. In particular, it helps to reduce the risks of hyperglycemia and hypoglycemia (Kesavadev et al., 2020). Insulin-only systems help stop the inflow of insulin when the level of sugar is below the needed threshold, while dual-hormone systems release glucagon when needed (Peters & Haidar, 2018). The second benefit is that the device constantly monitors the level of glucose in the blood, which may be crucial for doctors that provide care to the patient (Namikawa et al., 2018). Apart from these two benefits for patients’ health, the artificial pancreas also helps to increase their quality of life by improving their lifestyle flexibility (Schipp et al., 2022). The artificial pancreas is easier to use in comparison with insulin syringes, insulin pens, and insulin pumps (Kesavadev et al., 2020).
Creative applications of the artificial pancreas are hardly possible, as it serves a clear purpose. However, in the future, the device may be modified to monitor levels of other hormones or micro-elements in the body. For instance, it can measure the level of iron and inject it when needed to prevent anemia.
References
Boughton, C. K., & Hovorka, R. (2019). Is an artificial pancreas (closed‐loop system) for Type 1 diabetes effective? Diabetic Medicine, 36(3), 279-286.
Grigolon, R. B., Brietzke, E., Mansur, R. B., Idzikowski, M. A., Gerchman, F., De Felice, F. G., & McIntyre, R. S. (2019). Association between diabetes and mood disorders and the potential use of anti-hyperglycemic agents as antidepressants. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 95, 109720.
JDRF. (2017). How do people feel about using artificial pancreas technology?
Kesavadev, J., Saboo, B., Krishna, M. B., & Krishnan, G. (2020). Evolution of insulin delivery devices: from syringes, pens, and pumps to DIY artificial pancreas. Diabetes Therapy, 11(6), 1251-1269.
Namikawa, T., Munekage, M., Yatabe, T., Kitagawa, H., & Hanazaki, K. (2018). Current status and issues of the artificial pancreas: abridged English translation of a special issue in Japanese. Journal of Artificial Organs, 21(2), 132-137.
Peters, T. M., & Haidar, A. (2018). Dual‐hormone artificial pancreas: Benefits and limitations compared with single‐hormone systems. Diabetic Medicine, 35(4), 450-459.
Reaven, P. D., Emanuele, N. V., Wiitala, W. L., Bahn, G. D., Reda, D. J., McCarren, M.,… & Hayward, R. A. (2019). Intensive glucose control in patients with type 2 diabetes—15-year follow-up. New England Journal of Medicine, 380(23), 2215-2224.
Schipp, J., Skinner, T. C., Holloway, E., Scibilia, R., Langstrup, H., Speight, J., & Hendrieckx, C. (2022). ‘We’re all on the same team’. Perspectives on the future of artificial pancreas systems by adults in Australia with type 1 diabetes using open‐source technologies: A qualitative study. Diabetic Medicine, 39(5), e14708.
Szablewski, L. (2020). Blood Glucose Levels. IntechOpen.
